Journal of the Open Therapy Institute
Issue 2 | September 2025
Editorial Board
Andrew Hartz, PhD (Co-Editor in Chief) — Open Therapy Institute
Val Thomas, DPsych (Co-Editor in Chief) — Critical Therapy Antidote
Nafees Alam, PhD — University of Nebraska
Lawrence Amsel, MD, MPH — Columbia University
Joshua Aronson, PhD — New York University
Omar Sultan Haque, MD, PhD — Harvard University
Neil J. Kressel, PhD — William Paterson University
Dean McKay, PhD — Fordham University
Richard J. McNally, PhD — Harvard University
Pamela Paresky, PhD — Harvard University
Richard Redding, JD, PhD — Chapman University
Sally Satel, MD — Yale University
Michael Strambler, PhD — Yale University
Table of Contents
Introduction: The Emerging Movement | Andrew Hartz, PhD & Val Thomas, DPsych, Co-Editors in Chief
New Clinical Challenges
Self-Censorship Is Becoming a Mental Health Crisis | Chloe Carmichael, PhD
How Intensive Parenting Damages Childhood Mental Health | Camilo Ortiz, PhD and Matthew Fastman, PsyD
New Anxieties: The Fear of Being Cancelled | Dean McKay, PhD
Recovery from Transition: Psychotherapy with Detransitioners | Stella O’Malley, MA
Navigating Political Polarization with Individuals, Couples and Families | Linda Chamberlain, PsyD and William McCown, PhD
Overlooked Populations
Biases Against Men in Couples Therapy | Nafees Alam, PhD
Improving Mental Health Care for Police Officers | Kristopher Kaliebe, MD
Treating Patients Impacted by Anti-White Racial Aggression | Jaco van Zyl, MA
How Therapists Often Fail Religious Clients | Neil J. Kressel, PhD
Black Sheep and Double Binds: Treating Minorities with Heterodox Viewpoints | Lawrence Ian Reed, PhD
Biases in the Field
Why Therapy with Men Must Recognize Biological Sex Differences | William C. Sanderson, PhD
How Socio-Political Values Shape the Therapeutic Alliance | Nina Silander, PsyD
Cultural Misunderstandings: On the Misuses of the Term “Culture” | Douglas Novotny, PhD
Codifying Bias: How Activist Politics Became Embedded in Social Work Standards and Practices | Nafees Alam, PhD
Introduction: The Emerging Movement
Over the past decade, we’ve seen politicized institutions profoundly impact people’s lives, such as with speech codes, hiring discrimination, and ideological training in schools and the workplace. Marriages have ended, friendships have been broken, and family members are estranged. It’s clear that people care deeply about political issues and are significantly impacted by them. It’s also clear that people have great difficulty talking about these issues productively. These topics can lead to emotion dysregulation, interpersonal conflict, cognitive distortions, defense mechanisms, and even symptoms of mental illness.
Sadly, at a time when psychotherapy professions could be helpful for people with these issues, the field has succumbed to the same politicized dynamics that have occurred elsewhere, including shutting down dialogue, promoting activism over patient-centered care, and even pathologizing patients for their views or immutable characteristics. As a result, profound damage has been done to the profession, mistrust is at a high, and millions of patients are struggling to find a therapist who respects their values and understands their concerns.
Now, there seems to be an opening for dialogue and reform. As more people become tired of conflict, they’re looking for ways to move forward. This is an opportunity we shouldn’t miss, but correcting the field is an enormous undertaking. This involves more than just telling therapists to refrain from attacking their patients over politics; it requires helping therapists understand and empathize with the myriad groups of people they often ignore or view negatively.
Fortunately, these biases are finally being confronted. A dynamic and enterprising new professional community is emerging: a robust network of academics and practitioners committed to reform. They aren’t just exposing specific biases; they’re creating the institutional structures necessary to sustain lasting change. Frontiers in Mental Health is providing a platform for their pioneering work.
The second issue of this journal contains 14 new articles, each on an issue that affects countless people but is neglected because of the social political biases in the profession. Chloe Carmichael highlights how self-censorship damages mental health. Jaco van Zyl explores the common but almost entirely avoided topic of anti-white racial aggression, and Dean McKay describes the increasing prominence of a new type of anxiety disorder that focuses on the fear of being canceled. Each article offers insights and evidence and highlights areas where more research and more clinical resources are needed.
Several articles deal with couples’ and family issues. Nafees Alam identifies biases against men in couples’ therapy. Camilo Ortiz and Mathew Fastman discuss the myriad costs associated with intensive parenting, while Linda Chamberlain and William McCrown consider how political conflicts impact families.
Other populations that often encounter bias include: police officers (Kristopher Kaliebe), religious patients (Neil Kressel), detransitioners (Stella O’Malley), and various minority group members who have heterodox beliefs (Lawrence Ian Reed). Finally, several articles discuss broader biases in the profession, such as the problem of ignoring biological sex differences (William Sanderson), the importance of socio-political values for the therapeutic alliance (Nina Silander), the misuse of the term “culture” inside and outside the mental health profession (Douglas Novotny), and biases that have become codified in the social work profession (Nafees Alam).
Each of these topics has the potential to grow into a substantial research program or clinical specialty in its own right. These articles are intended to start conversations, not end them. Further research, training, and service improvements are needed on each. Hopefully, these authors’ insights will serve as a catalyst to spark broader research, enhance training, and improve therapeutic services for millions of people.
— Andrew Hartz, PhD & Val Thomas, DPsych, Co-Editors in Chief
Self-Censorship Is Becoming a Mental Health Crisis
By Chloe Carmichael, PhD
More and more, therapy clients are arriving not with buried childhood traumas or abstract existential worries, but with a simple, gnawing problem: they’re afraid to speak their minds. It’s not stage fright or fear of public speaking. It’s the quiet, chronic fear of saying the wrong thing in a conversation with a friend, coworker, or family member and facing social or professional consequences. What we’re witnessing is more than a political or cultural shift—it’s a mental health trend.
As a clinical psychologist, I’ve seen how internal gag orders, whether imposed by political polarization, fear of mislabeling, or cultural confusion over what counts as “harmful speech,” can erode a person’s mental clarity, self-trust, and relationships. Free speech is not just a legal issue—it’s a psychological one, and the effects of suppressing it are showing up in therapy rooms across the country.
How Self-Censorship Shows Up in Mental Health Treatment
Fear of speaking up, rooted in social pressure, manifests in therapy in subtle but damaging ways. Clients describe withholding their opinions on sensitive topics, even from their therapists, for fear of judgment (Blanchard & Farber, 2015). Others share that they nod along in conversations where they feel uncomfortable, repressing discomfort to maintain social harmony. Over time, this pattern of self-silencing can erode self-efficacy and self-esteem (Tran, 2024).
Clinical research underscores the psychological toll of chronic self-silencing. For example, research on reflective verbalization suggests that articulating thoughts—even privately through journaling (Zheng, Lu, & Gan, 2019)—can significantly enhance insight and problem-solving (Wetzstein & Hacker, 2004). Conversely, habitual suppression of one’s views in social interactions can lead to emotional numbing and diminished self-efficacy. Research also shows that emotionally charged conversations, such as those involving politics, which are common sources of personal strain for many clients, can activate automatic emotional responses, making it harder to process information rationally (Morris et al., 2003). This helps explain why many clients fear such discussions or freeze in moments of disagreement. The longer clients suppress their true thoughts and emotions, the harder it becomes to locate and express them authentically.
An example taken from my new book (Carmichael, 2025) involves a client who discovered through frank therapeutic conversation and journaling that his years of “going along to get along” at work had numbed his ability to grapple directly with anger about being excluded for promotions due to diversity, equity, and inclusion initiatives. He eventually stymied himself so much that he became repressed, stuck in denial and the inability to connect with much drive around his professional goals. He was introduced to journaling as a way of articulating and questioning his thoughts, and this practice allowed him to gradually regain his voice and respond to the people and situations in his life more authentically and effectively. Another client felt fraudulent in her relationship with a beloved and strongly opinionated aunt. This client hid her political views to avoid being ostracized; her aunt had made it clear that anyone who voted like my client was “dead to her.” She benefited from using a suite of techniques, including the two listed below. Both clients found relief through open speech and the acknowledgment that their silence had come at an emotional and cognitive cost.
Helpful Therapeutic Solutions
Helping clients navigate the fear of speaking up requires more than telling them to speak up. Many already want to but feel paralyzed. Therapists need some strategies at their disposal—in particular, structured, step-by-step tools. Two effective techniques that can be used in clinical practice are the WAIT test and Say Your Line (Carmichael, 2025).
The WAIT Test
WAIT stands for Want, Appropriate, Inoculate, Trust. It helps clients think through whether, when, and how to speak up. The client is given the following directions:
W—Want: Ask yourself, “Do I really want to speak up?” Not every situation requires a response. For instance, if you’re tired and drained at the end of a long day, it might be okay to let a comment slide. But if you feel your silence is eating at you later, it’s a sign that your authentic self wants to be heard.
A—Appropriate: Is this the right time and place? If you’re about to bring up a politically charged topic with your new partner, it may be better to do it over a quiet dinner than at a noisy gathering. Choose a setting that allows space for a meaningful exchange.
I—Inoculate: Give the other person a small dose of what you want to say before you go all in. This might sound like, “Hey, I’d like to share something that may be a little different than what you’re used to hearing, but I’m hoping we can talk about it openly.” This primes them to receive your point without feeling blindsided and gives you a chance to see how they react to you sharing a little bit before you dive in deeper.
T—Trust: Ask yourself: “Do I trust this person or at least trust myself to handle the fallout if the conversation doesn’t go well?” You may not be able to control how others respond, but you can decide that even if it’s hard, you’ll have your own back.
Using the WAIT test before entering a difficult conversation helps reduce impulsive speech driven by frustration or anxiety. It also builds confidence by showing clients that they have a plan.
Say Your Line
Sometimes the most challenging part of speaking up is just getting started. The Say Your Line technique helps clients overcome that first hurdle by focusing only on the opening sentence or two of a difficult conversation. It draws on the cognitive-behavioral therapy tool of cognitive rehearsal, but zeroes in on the moment of initiation. The client is directed step-by-step using the following instructions:
Choose your line: Think about what you want to say, then craft one or two simple sentences that express it clearly and calmly. For example: “Actually, I see it differently—would you like to know why?” or “There’s something I’ve been meaning to say that’s a little sensitive but important to me.”
Imagine you’re an actor: Instead of emotionally gearing up for a high-stakes confrontation, shift your mindset. Pretend you’re an actor whose only job is to deliver a line. This can help remove the emotional weight and make it easier to simply speak.
Practice out loud: Say the line aloud a few times in a neutral tone, like you’re rehearsing a part. This builds familiarity and reduces pressure.
Deliver it: When the moment comes, don’t try to think through the entire conversation. Just take a breath and say your line. Once you’ve begun, you can move naturally into the rest of the dialogue.
Say Your Line is ideal for clients who already feel reasonably prepared, but who freeze up at the starting gate. It offers a quick on-ramp into dialogue without needing to map out every possible outcome. For clients who have done deeper work (e.g., using the WAIT test), this technique helps put their preparation into motion.
Conclusion: Reclaiming Speech as a Mental Health Imperative
Speech is more than communication; it’s a cognitive and emotional lifeline. When we silence ourselves, especially habitually and around deeply held values, we risk compromising our mental health. Therapists have a role to play in naming this issue and offering tools to help clients reclaim their voices. Encouraging open dialogue, practicing self-awareness, and equipping clients with simple and effective techniques can foster both personal growth and relational healing.
In a time when many feel they must choose between silence and exile, reclaiming our voice isn’t just a therapeutic task—it’s a cultural imperative. Whether you’re in the therapy room or across the dinner table, the ability to speak openly, without fear of exile, is essential for personal well-being and a resilient society. This cultural silencing (Rudert et al., 2017) may also be one hidden contributor to the loneliness epidemic that public health leaders, including the U.S. Surgeon General, are urgently working to address.
References
Blanchard, M., & Farber, B. A. (2015). Lying in psychotherapy: Why and what clients don’t tell their therapist about therapy and their relationship. Counselling Psychology Quarterly, 29(1), 90–112. https://doi.org/10.1080/09515070.2015.1085365
Carmichael, C. (2025). Can I say that? Why free speech matters and how to use it fearlessly. Skyhorse Publishing.
Morris, J. P., Squires, N. K., Taber, C. S., & Lodge, M. (2003). Activation of political attitudes: A psychophysiological examination of the hot cognition hypothesis. Political Psychology, 24(4), 727–745. https://doi.org/10.1046/j.1467-9221.2003.00349.x
Rudert, S. C., Hales, A. H., Greifeneder, R., & Williams, K. D. (2017). When silence is not golden: Why acknowledgment matters even when being excluded. Personality and Social Psychology Bulletin, 43(5), 678–692. https://doi.org/10.1177/0146167217695554
Tran, C. (2024). Self-efficacy’s mediating role on the relationship between personality and depression in the unemployed [Master’s thesis, San José State University]. https://doi.org/10.31979/etd.gmg9-ykt5
Wetzstein, A. & Hacker, W. (2004). Reflective verbalization improves solutions—The effects of question‐based reflection in design problem solving. Applied Cognitive Psychology, 18(2): 145–56. https://doi.org/10.1002/acp.949
Zheng, L., Lu, Q., & Gan, Y. (2019). Effects of expressive writing and use of cognitive words on meaning making and post-traumatic growth. Journal of Pacific Rim Psychology, 13, e5. https://doi.org/10.1017/prp.2018.31
How Intensive Parenting Damages Childhood Mental Health
By Camilo Ortiz, PhD and Matthew Fastman, PsyD
Parenting styles have shifted radically over the past few decades. But as parents spend more time with their children and pay more attention to their mental health, rates of childhood mental illness appear to be skyrocketing. How could this be? One possibility is that over-intensive parenting deprives children of opportunities to explore and build competence. While this approach to parenting is well-intentioned, it typically leaves parents exhausted and kids fragile and immature. This paper will outline this problem and propose solutions for both parents and therapists.
Background
Research indicates that parents have spent significantly more time with their children since the 1990s. For example, today’s working mothers spend as much time with children as stay-at-home mothers did in 1975. Such quantitative investigations align with qualitative reports of parents adopting more controlling behaviors, particularly among middle- and upper-class families.
This shift in child rearing, commonly referred to as helicopter parenting or parental overinvolvement, can be defined as a parenting style characterized by excessive participation in most of a child’s decisions, including those where parental action is inappropriate given the child’s level of development. Research suggests that overinvolved parenting is associated with poorer autonomy development, self-efficacy, and emotional regulation in children (Segrin et al., 2013).
There are several subtypes of overinvolved parents, the most common being the anxious-overinvolved subtype. Anxious parents are prone to overparenting because they often have heightened perceptions of risk, which leads to restrictive parenting, including less willingness to allow their children to play alone (Aziz & Said, 2012). A high trait level of anxiety can cause greater relief for that parent when they intervene. In other words, it is more rewarding for anxious parents to intervene because of the outsized relief they feel.
Parental overinvolvement can affect children in several ways, such as by modeling avoidance for their children. These behaviors could include:
By avoiding anxiety-provoking situations, parents may teach their children to behave similarly through vicarious learning.
Anxious parents are also prone to accommodate children’s avoidance of difficult or anxiety-provoking tasks. Parental accommodation may facilitate children’s avoidance and safety behaviors by providing reassurance and validation and doing what children are afraid of for them.
Parental accommodation of child anxiety can include preemptive accommodations that are meant to help a child avoid anxiety-inducing situations (e.g., avoiding drop-off playdates for a child with separation anxiety), or they can include reactive accommodations that are intended to help a child escape an anxiety-inducing situation (e.g., ordering ice cream for a child who is afraid to walk up to the counter and order himself). While the relationship between parental accommodation and child anxiety appears to be bidirectional, it is also clear that these well-intentioned parental responses reinforce maladaptive coping mechanisms, impede corrective learning, and sustain elevated anxiety sensitivity (Lebowitz et al., 2015). The resulting short-term anxiety reduction of accommodation reinforces further dependence and avoidance in children, thus maintaining anxiety symptoms.
How Intrusive Parenting Shows Up in Psychological Clinics
The effects of overinvolved parenting on children can be widespread and profound. Parental overinvolvement is positively associated with anxiety severity in children (Rapee, 1997). Children of overinvolved parents are given fewer opportunities to handle challenging experiences independently, which in turn limits their ability to develop coping and problem-solving skills. This may increase their belief that they cannot tolerate stress and discomfort (Segrin et al., 2013). These skill deficits can turn normative childhood challenges into more serious mental health problems, as anxious avoidance can quickly feed on itself and rapidly increase in seriousness. For example, children who have normative and even healthy anxiety of speaking to strangers may begin to refuse all interactions with strangers, such as the parents of friends, extended family, and school personnel. These children may present for professional intervention when avoidance begins to interfere with functioning, such as in the case of school avoidance.
How Can Psychologists Provide Solutions?
Two psychological approaches for child anxiety have been demonstrated to be effective. The first, exposure therapy with blocked escape (Kendall et al., 2005), involves repeatedly facing feared stimuli and is meant to deliberately violate negative expectancies of harm, decontextualize inhibitory associations, and increase tolerance of distress (Craske et al., 2008). The second, parent accommodation-based approaches, such as Supportive Parenting for Anxious Childhood Emotions (SPACE; Lebowitz et al., 2020), are meant to block parental involvement in reducing manageable child anxiety. Both approaches can be challenging for parents, particularly those who are concerned about seeing distress in their children. Children also commonly exhibit extinction bursts, which are behavioral and emotional escalations when parents set limits on accommodation. For example, children often throw tantrums if a parent attempts to prompt them to sleep in their own bed for the night, which can lead a parent to withdraw the directive. This can have the paradoxical effect of increasing parental accommodations to secure short-term relief from the child’s escalation.
A new treatment for child anxiety, Independence-Focused Therapy (IFT), targets overparenting by leveraging children’s universal desire to do things independently (Ortiz & Fastman, 2024). In this treatment, children indicate which independence activities (IAs), such as riding a bike to the park alone, shopping for food alone, and taking a train alone, they would like to do. Parents are not present during IAs and, therefore, cannot intrusively intervene. Recent compelling evidence suggests that exposure therapy has beneficial effects on stimuli that are not even in the same fear category as the fears being targeted. For example, exposure to spiders improved anxiety of heights in participants who had phobias of both (Kodzaga et al., 2023). It is precisely this dissimilarity that may make IAs more acceptable to children, their parents, and clinicians. For example, a child with a fear of the dark who is allowed to ride his bike to the park alone may experience a reduction in his fear without ever directly exposing him to the dark. This is due to the shared underlying mechanisms operating in both cases. Preliminary data suggest that daily IAs lead to less anxiety in children and greater confidence by their parents that they are capable. Recent data (Inserra & Ortiz, 2025) found that parents reported IFT to be equally acceptable as a treatment to traditional cognitive-behavioral therapy. Further research is needed to examine the long-term effects of IFT and moderators on treatment outcomes.
Conclusion
The rise of intensive or overinvolved parenting appears to be an important cause of rapidly increasing rates of child anxiety. Evidence-based approaches, such as exposure therapy and reducing parental accommodations, are insufficient to reverse this troubling increase. Novel approaches, such as IFT, that are rapidly scalable and have lower training requirements, are a promising approach to help these children and their parents.
References
Aziz, S., & Said, A. (2012). Parental anxiety and risk perception: Implications for restrictive parenting. Journal of Child and Family Studies, 21(6), 950–958. https://doi.org/10.1007/s10826-012-9567-3
Craske, M. G., Kircanski, K., Zelikowsky, M., Mystkowski, J., Chowdhury, N., & Baker, A. (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46(1), 5–27. https://doi.org/10.1016/j.brat.2007.10.003
Inserra, A., & Ortiz, C. (2025). Treatment acceptability of independence-focused therapy and exposure therapy [Unpublished doctoral dissertation]. Long Island University-Post.
Kendall, P. C., Hudson, J. L., Gosch, E., Flannery-Schroeder, E., & Suveg, C. (2005). Cognitive-behavioral therapy for anxiety-disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology, 73(1), 135–147. https://doi.org/10.1037/0022-006X.73.1.135
Kodzaga, I., Dere, E., & Zlomuzica, A. (2023). Generalization of beneficial exposure effects to untreated stimuli from another fear category. Translational Psychiatry, 13(1), 401. https://doi.org/10.1038/s41398-023-02698-7
Lebowitz, E. R., Marin, C., Martino, A., Shimshoni, Y., & Silverman, W. K. (2020). Parent-based treatment as efficacious as cognitive-behavioral therapy for childhood anxiety: A randomized noninferiority study of supportive parenting for anxious childhood emotions. Journal of the American Academy of Child & Adolescent Psychiatry, 59(3), 362–372. https://doi.org/10.1016/j.jaac.2019.02.014
Lebowitz, E. R., Scharfstein, L. A., & Jones, J. (2015). Comparing family accommodation in pediatric obsessive-compulsive disorder, anxiety disorders, and non-anxious children. Depression and Anxiety, 32(12), 908–916. https://doi.org/10.1002/da.22451
Ortiz, C., & Fastman, M. (2024). A novel independence intervention to treat child anxiety: A nonconcurrent multiple baseline evaluation. Journal of Anxiety Disorders, 105, Article 102893. https://doi.org/10.1016/j.janxdis.2024.102893
Rapee, R. M. (1997). Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review, 17(1), 47–67. https://doi.org/10.1016/S0272-7358(96)00040-2
Segrin, C., Woszidlo, A., Givertz, M., & Montgomery, N. (2013). Parent and child traits associated with overparenting. Journal of Social and Clinical Psychology, 32(6), 569–595. https://doi.org/10.1521/jscp.2013.32.6.569
New Anxieties: The Fear of Being Cancelled
By Dean McKay, PhD
Akyrono (ακυρώνω )—from Greek, meaning “to nullify”
As society becomes increasingly polarized, people are being pressured to align themselves publicly with the currently accepted political narrative. It is not surprising that self-reported anxiety states are rising. In this essay, I will be arguing that these punishing social conditions are now in danger of generating new mental health disorders. In this essay, I argue that one particular anxiety disorder variant is becoming apparent, characterized by an irrational fear of being canceled. I am therefore naming this “akyró̱no̱phobia,” derived from the Greek meaning “to nullify.”
Anxiety disorders are highly prevalent in the general public, with estimates suggesting that close to 20% of the public will have had serious anxiety within the past year and that just over 34% will experience it during their lifetimes (Szuhany & Simon, 2022). Although the current diagnostic manual lists obsessive-compulsive disorder (OCD) in a separate category, that condition is also marked by significant anxiety and afflicts around 2% of the population (Pampaloni et al., 2022). Collectively, this means that approximately 66 million Americans will suffer from an anxiety disorder or OCD in the next year.
Experts in anxiety disorders and OCD have begun to recognize a specific manifestation, marked by intense and exaggerated fears of being canceled. I recently engaged colleagues on an expert network regarding how frequently they have treated individuals with fears of being canceled. This informal polling showed that of 187 colleagues, 147 reported anywhere from two cases to dozens who report this specific fear. The symptoms associated with this fear have included such diverse behaviors as avoiding social interactions and online conversations, destroying emails received from others if the individual remotely suspects it has upsetting content, and seeking reassurance from past consensual sexual partners that their intimacy was, in fact, appropriate. This is not an exhaustive list, but one common thread is that the sufferers generally possess personal qualities that make them particularly low risk for committing any act that might be deemed suitable for cancelation in the online social ecosystem. Specifically, most people with OCD typically have higher levels of neuroticism, a personality trait that makes people risk-averse (Barlow et al., 2014).
The Nature of Akyró̱no̱phobia
In proposing this phobia, it is reasonable to suggest it is characterized by two different patterns of psychopathology. One pattern may be obsessive-compulsive thoughts about the risk of cancelation and compulsive behaviors to ward off these risks. The other may be generalized anxiety, with worries about actions that might result in cancelation, with a dominant anxious mood and associated physical consequences (i.e., muscle tension or gastrointestinal distress).
Considering the high-profile figures who have been canceled, it is little surprise that individuals prone to experiencing anxiety would suffer fears of it happening to them. To illustrate, if one were to simply Google the search term “people who were canceled,” it results in lists of public figures who were canceled stratified by year. It is such a pervasive social phenomenon that it is annually summarized. The manifestation of most anxiety conditions is embedded in the social context in which people live. The nature of akyró̱no̱phobia may be categorized into two different types.
Obsessive-Compulsive Type Akyró̱no̱phobia
Obsessions are characterized as intrusive and unwanted thoughts that the sufferer recognizes as irrational. These thoughts lead to considerable avoidance of situations that might provoke them and may or may not result in compulsive behaviors. Research has shown that OCD is highly heterogeneous, marked by subtypes (McKay et al., 2004; Wheaton et al., 2015). One facet of OCD that makes it a condition highly susceptible to akyró̱no̱phobia is that obsessions are typically a result of socially unacceptable ideas or situations that are widely held concerns by the public. To illustrate, whenever a serious illness gets media attention (such as COVID-19), individuals with OCD are more likely to express extreme concerns over contracting that condition (Sheu, McKay, & Storch, 2020).
This means that the social milieu is ripe terrain for obsessional content. When public figures face cancelation, experts in OCD can (and do) expect to see clients reporting intrusive thoughts that the same fate may await them. These individuals suffer greatly, as the offenses that drive their obsessions are very minor and would not be considered offenses for most. For example, in my anecdotal poll of colleagues, one commented that it was not uncommon for clients they had treated to scrub their computers of any emails they received that they thought might contain slightly offensive content. Some severe cases have even involved avoiding people out of concern that they might have an offensive thought in their presence. All of these obsessions are for thoughts, with no intent to commit any even remotely offensive actions or to utter any offensive remarks.
Generalized Anxiety Type Akyró̱no̱phobia
While obsessions over the risk of acting on offensive and unwanted thoughts is a well-known variant of OCD, akyró̱no̱phobia can also prompt serious worries that are associated with generalized anxiety disorder (GAD). Unlike OCD, the concerns associated with akyró̱no̱phobia are marked by reviewing past statements, emails, social media posts, and other public comments for the slightest potential for offending content. As with any worries, a prevailing challenge for sufferers is intolerance of uncertainty (Jacoby, 2020). The pain of this variation of akyró̱no̱phobia is that individuals can point to specific acts that they interpret as potentially offensive, connect these to acts of other public figures, and claim that their offenses are on par with the ones that resulted in others being canceled.
Treatment, Policy, and Politics
The above illustrations of how cancel culture can result in significant OCD or GAD manifestations that I have termed akyró̱no̱phobia should be viewed as cautionary tales of how public discourse and mob-inspired desires for retribution can inflict pain and suffering indirectly on innocent individuals. It also should be considered an area where redress is possible.
On a granular level, people with akyró̱no̱phobia can benefit from existing treatment approaches, so long as these are used with care. Exposure therapy is commonly prescribed for fears and OCD, and akyró̱no̱phobia would be no exception. It is essential that specific attention be given to social forces to ensure exposure is conducted not only ethically but also safely in the current social climate (as discussed in the context of COVID-19-related exposure in Sheu, McKay, & Storch, 2020).
On a policy level, mental health professional organizations would do well to consider the extent to which their policies genuinely embrace pluralism. In my anecdotal poll of colleagues, several also cited prevailing attitudes among colleagues as potentially making clients feel less comfortable expressing putative offensive thoughts to their clinicians. Reorienting the profession to accept clients for the full range of ordinary human emotional and cognitive experiences will go a long way toward addressing this issue.
As for politics, the mental health professions can do far better in embracing pluralism as well. This would mean endorsing a sense of fairness for all and setting aside some troubling movements that would allow clinicians to issue judgments about how clients may or may not receive care (McKay & White, in press; Strambler, in press). The mental health professions can and should do better to prevent unwanted and painful anxiety conditions. Addressing the illiberal excesses of cancel culture would be a significant public health benefit.
A Look Ahead
The public is generally unaware of this, but the mental health professions are collectively engaged in an internal struggle over how to address politics, both during within-session discussions with clients and concerning the policies they establish for professional conduct. The presence of akyró̱no̱phobia illustrates one of many places where clinicians lack clear guidance in how to best proceed, given the political focus within the profession. There is a growing recognition that political processes in the profession have been unrestrained and have lacked clear guidelines. For example, there have been increasing concerns that the politicization of the American Psychological Association has led professional members of the profession to hold anti-Semitic attitudes that emerge from anti-Zionist political viewpoints. There have been calls within some mental health professional communities to explicitly screen clients for political views and reject those who hold positions contrary to clinicians. These two examples only scratch the surface and represent ill-formed and heavy-handed attempts to integrate political processes into professional activities. This is hardly surprising since mental health professionals are not formally trained in political discourse. It is hoped that as the professions effectively address this challenge, there may correspondingly be attention paid to akyró̱no̱phobia in a non-judgmental manner, allowing clinicians to feel less constrained in addressing the individual needs of clients who report this problem.
References
Barlow, D.H., Sauer-Zavala, S., Carl, J.R., Bullis, J.R., & Ellard, K.K. (2014). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2, 344–365. https://doi.org/10.1177/2167702613505532
Jacoby, R.J. (2020). Intolerance of uncertainty. In J.S. Abramowitz & S.M. Blakey (Eds.), Clinical handbook of fear and anxiety: Maintenance processes and treatment mechanisms (pp. 45–63). American Psychological Association.
McKay, D., Abramowitz, J., Calamari, J., Kyrios, M., Radomsky, A., Sookman, D., Taylor, S., & Wilhelm, S. (2004). A critical evaluation of obsessive-compulsive disorder subtypes: Symptoms versus mechanisms. Clinical Psychology Review, 24, 283–313. https://doi.org/10.1016/j.cpr.2004.04.003
McKay, D., & White, E.K. (in press). Philosophical errors and unintended harms in recrafting the foundation of counseling and psychotherapy: Comment on Sue, Neville & Smith (2024). American Psychologist.
Pampaloni, I., Marriott, S., Pessina, E., Fisher, C., Govender, A., Mohamed, H., Chandler, A., Tyagi, H., Morris, L., & Pallanti, S. (2022). The global assessment of OCD. Comprehensive Psychiatry, 118. https://doi.org/10.1016/j.comppsych.2022.152342
Sheu, J.C., McKay, D., & Storch, E.A. (2020). COVID-19 and OCD: Potential impact of exposure and response prevention therapy. Journal of Anxiety Disorders, 76. https://doi.org/10.1016/j.janxdis.2020.102314
Strambler, M.J. (in press). Universalism is not white: Commentary on Sue et al. (2024). American Psychologist.
Szuhany, K.L., & Simon, N.M. (2022). Anxiety disorders: A review. JAMA, 328, 2431–2445. https://doi.org/10.47191/ijcsrr/V7-i7-53
Wheaton, M.G., Schwartz, M.R., Pascucci, O., & Simpson, H.B. (2015). Cognitive-behavior therapy outcomes for obsessive-compulsive disorder: Exposure with response prevention. Psychiatric Annals, 45, 303–307. https://doi.org/10.3928/00485713-20150602-05
Recovery from Transition: Psychotherapy with Detransitioners
By Stella O’Malley, MA
Over the past decade, gender dysphoria has emerged as one of the most complex and sensitive issues facing young people, families, and clinicians. There has been a sharp rise in adolescents seeking support for gender-related distress (Cass, 2024; Chen et al., 2016; Olson-Kennedy et al., 2016). Related to this change, many therapists report an overwhelming demand for thoughtful, well-informed therapy in this area and a dearth of providers offering it.
Since 2017, I’ve worked as a therapist and support group facilitator for families, detransitioners, transgender individuals, and those experiencing distress following medical transition. I’ve regularly met with individuals who feel isolated, regretful, and let down by the very systems that were supposed to help them. Despite the growing need for services, though, many therapists avoid this work due to political pressure and concerns about professional risks. Therefore, access to psychological care remains limited.
There is currently a tremendous need for services that provide non-medicalized, evidence-based approaches to gender-related distress. Patients struggling with these concerns should always be met with curiosity, compassion, and clinical integrity (Clark et al., 2024). Of course, these same principles apply to treatment with detransitioners and others experiencing distress related to a medical gender transition.
Increasing Numbers of Detransitioners
The decision to detransition often comes after years of psychological struggle, with many facing heightened suicidality during this uncertain stage. Social rejection and isolation are common, compounding the emotional burden (Vandenbussche, 2022).
Detransition appears to be on the rise, possibly due to the increase in medical transitions or the influence of the gender-affirming model, which is patient-led and centers on self-identification, often resulting in medical intervention (WPATH, 2022). However, limited research makes it difficult to determine precise causes.
As one piece of evidence, the Reddit forum r/detrans (which features stories, questions, and resources about detransitioning) had fewer than 1,000 members in 2019; today, it has over 57,000. Media reports now frequently feature detransitioners whose stories often involve regret, isolation, and irreversible medical outcomes (see below). These experiences demand greater attention from clinicians, researchers, and policymakers alike.
Vandenbussche (2022) surveyed 237 detransitioners and desisters—92% female and 8% male—recruited from online communities. Desisters are those who no longer identify as transgender without undergoing medical transition, while detransitioners have medically transitioned and later reversed their course. The study found that 70% attributed their gender dysphoria to underlying issues such as mental health struggles, trauma, or internalized homophobia, and many felt that they had been inadequately informed about the treatments they received.
Stories of detransition and desisting are compelling. Psychoanalyst Lisa Marchiano (2021) documented the case of Maya, a distressed adolescent with an eating disorder who underwent medical transition and later detransitioned. In the same article, Marchiano referenced Livia, a woman who regretted transitioning after undergoing a mastectomy at 20 and a hysterectomy at 21.
Similarly, Reuters (Respaut et al., 2022) profiled Max Lazzara. At 14, Max began questioning her gender identity and found affirmation through online communities. By 16, she had started testosterone, and at 18, she underwent a mastectomy. Although she initially felt relief, her mental health deteriorated further, resulting in renewed suicide attempts, substance abuse, and disordered eating. In 2020, she came to identify as a lesbian, ceased testosterone, and now regrets that medicalization was offered as the answer to her distress.
Meanwhile, the New York Times (Paul, 2024) recounts the story of Grace Powell, who, as a teenager, believed transition would resolve her distress over puberty, bullying, and depression. She began cross-sex hormones at 17 and later had a double mastectomy. Yet, no one explored her underlying issues, including past trauma, before affirming her transition. She has since detransitioned and expresses regret.
Paul also profiles Kasey Emerick, who grew up in a conservative Christian community and transitioned to escape the stigma of being a lesbian. After five years living as a trans man, Emerick realized her mental health had worsened, detransitioned in 2022, and faced intense online backlash.
Littman (2021) found that 55% of 100 detransitioners reported inadequate evaluation before transitioning, 38% linked their dysphoria to trauma, abuse, or mental health issues, and 23% cited homophobia or difficulty accepting their sexual orientation as contributing factors in both transitioning and detransitioning. Similarly, Vandenbussche (2022) reported that 52% of detransitioners and desisters expressed a need to cope with internalized homophobia. These findings highlight the importance of addressing underlying psychological issues in therapy, rather than reinforcing the belief that medical transition is the only path forward. However, internalized homophobia is just one of many challenges detransitioners face. Unacknowledged comorbidities also pose significant barriers to recovery and wellbeing.
Challenges Facing Detransitioners
My work with detransitioners has been some of the most meaningful, and at times harrowing, of my career. The individuals I’ve worked with typically view their medical transition as a form of self-harm and deeply regret the hormonal and surgical interventions they underwent, highlighting the potential risks of medicalization.
I regularly hear from individuals who deeply regret undergoing hormonal treatments, mastectomies, vaginoplasties, hysterectomies, and other irreversible procedures. Detransitioners remain a minority within a minority, and yet their voices must be heard to fully understand the realities of gender dysphoria.
The consistent stories I encounter underscore the urgent need to approach gender dysphoria with caution, compassion, and a focus on long-term wellbeing (Littman et al., 2021, 2024; O’Malley & Bell, 2024). Internalized and externalized homophobia is a recurring theme in my clinical work. Many young people who later identify as gay, lesbian, or bisexual describe struggling to accept their same-sex attraction and now regret pursuing medical transition as a way to “trans the gay away,” a phrase commonly used online to describe this phenomenon.
Physical complications from medical transition are a constant source of distress for group participants. Pain, incontinence, osteoporosis, and cardiac issues are frequently mentioned. Along with deep regret over harmful medical interventions and sadness over lost years, these challenges create an almost unbearable burden. The age range of participants is striking, spanning from 18 to 85 years old.
Conclusion
As awareness of detransition grows, so too must our willingness to listen without defensiveness or ideological bias. Those who regret their medical transition are not anomalies or statistics; they are people whose experiences expose critical gaps in our clinical practices, health care systems, and cultural assumptions.
We owe it to these individuals to take their experiences seriously. This means investing in robust psychological support, ensuring proper assessment and informed consent, and creating space for identity exploration without rushing to medicalization. Above all, this role requires compassion—not just for those who transition, but also for those who choose a different path.
References
Cass, H. (2024). Independent review of gender identity services for children and young people. The Cass Review. https://cass.independent-review.uk/home/publications/final-report/
Chen, M., Fuqua, J., & Eugster, E. A. (2016). Characteristics of referrals for gender dysphoria over a 13-year period. Journal of Adolescent Health, 58, 369–371. https://doi.org/10.1016/j.jadohealth.2015.11.010
Clark, C., Pluckrose, H., O’Malley, S., & Miller, A. (2024, November 13). Our position FAQs. Genspect. https://genspect.org/our-position-faqs/
Littman, L. (2021). Individuals treated for gender dysphoria with medical and/or surgical transition who subsequently detransitioned: A survey of 100 detransitioners. Archives of Sexual Behavior, 50(8), 3353–3369. https://doi.org/10.1007/s10508-021-02163-w
Marchiano, L. (2021). Gender detransition: A case study. Journal of Analytical Psychology, 66(4), 813–832. https://doi.org/10.1111/1468-5922.12711
Olson-Kennedy, J., Cohen-Kettenis, P. T., Kreukels, B. P. C., Meyer-Bahlburg, H. F. L., Garofalo, R., Meyer, W., & Rosenthal, S. M. (2016). Research priorities for gender nonconforming/transgender youth: Gender identity development and biopsychosocial outcomes. Current Opinion in Endocrinology, Diabetes, and Obesity, 23, 172–179. https://doi.org/10.1097/MED.0000000000000236
O’Malley, S. & Bell, K. (2024, March 12). We need to complexify our understanding of transition and detransition. Genspect. https://genspect.org/we-need-to-complexify-our-understanding-of-transition-and-detransition/
Paul, P. (2024, February 2). As kids, they thought they were trans. They no longer do. The New York Times. https://www.nytimes.com/2024/02/02/opinion/transgender-children-gender-dysphoria.html
Respaut, R., Terhune, C., & Conlin, M. (2022, December 22). Why detransitioners are crucial to the science of gender care. Reuters. https://www.reuters.com/investigates/special-report/usa-transyouth-outcomes/.
Vandenbussche, E. (2022). Detransition-related needs and support: A cross-sectional online survey. Journal of Homosexuality, 69(9), 1602–1620. https://doi.org/10.1080/00918369.2021.1919479
World Professional Association for Transgender Health. (2022). Standards of care for the health of transgender and gender diverse people (Version 8). WPATH. https://www.wpath.org/publications/soc8/
Navigating Political Polarization with Individuals, Couples and Families
By Linda Chamberlain, PsyD and William McCown, PhD
Mental health professionals are increasingly confronted with the impact of political polarization on our clients’ most important relationships. Therapists are faced with how partisanship is straining family bonds: Clients cancel holiday gatherings, avoid dating people with opposing views, and endure long-term estrangements over ideological differences. As these issues surface in clinical settings, mental health professionals must be equipped to navigate the relational damage caused by political polarization. What can we do to help?
The Family System Under Stress
“My fiancé broke off our engagement. She knows I’m a conservative, but we got in a huge argument about deporting illegal immigrants, and she lost her mind. She called me a racist and colonizer, whatever that means. She’s been getting more radical about her liberal beliefs, and it’s finally wrecked our relationship. This feels so unfair.” (28-year-old male)
Finding a person to date has always been challenging, and the ideological divide between men and women adds to the complexity of this issue. We know that over the last few decades, men have tended to lean toward the Republican Party (52%), while women have leaned toward the Democratic Party (51%) (Pew Research Center, 2024). This small gap, however, is becoming a canyon. The gender divide is even more pronounced in Gen Z (born 1997–2012), with women becoming significantly more liberal and men becoming somewhat more conservative (Yale University, 2025).
Increasingly, couples who don’t share a political orientation are challenged to negotiate their differences or experience deep divides in their relationship, potentially resulting in separation.
“We finally stopped going out socially with our friends. Someone would always bring up something political, and we would get into an argument with each other. Now, we mostly sit in separate rooms at home watching different news stations or see our friends separately. I don’t want this.” (Wife married 24 years)
The impact of political discord extends beyond couples. Parent-child estrangements are increasingly common, with political disagreements sometimes acting as stand-ins for deeper emotional rifts.
“I just can’t believe that my mother voted for that man! It’s like she was blinded and couldn’t see who he is. I can’t be around her. That’s lasted for two years, and I can’t seem to forgive her.” (24-year-old female college student)
Sibling relationships are particularly vulnerable, with partisanship exacerbating long-standing rivalries and differences. Politics is second only to conflicts over aging parents and inheritances in destroying sibling bonds (Safer, 2019). Political conflict often masks unresolved issues such as parental favoritism or divergent values that require therapeutic investigation.
Extended families are also fracturing under political stress. Even minor conversations about current events can escalate into personal attacks and mutual recriminations. Clients report dread over holiday gatherings, with some choosing isolation over potential confrontation. During the 2024 holiday season, more than seven out of 10 adults surveyed said they hoped to avoid political discussions with family members (APA, 2024). In response, a plethora of advice has appeared very recently on internet platforms, usually taking the form of pragmatic tips to avoid potential conflict.
Effective Therapeutic Approaches
In this landscape of heightened division, it is crucial for psychotherapists to work skillfully with clients whose lives are impacted by political polarization. Navigating these tensions in the therapy room requires sensitivity, adaptability, and a nonjudgmental stance, as political differences often serve as proxies for deeper relational wounds or unmet needs. A fierce argument that flares up about the imposition of tariffs, for example, may have little to do with the matter itself, but instead operates as a channel for childhood grievances about perceived favoritism within the family.
By fostering an environment where clients feel safe to explore their values and emotional responses without fear of invalidation or escalation, therapists empower individuals and families to develop empathy, resilience, and authentic connection. This work not only eases relational distress but also equips clients to engage more thoughtfully in a polarized world, promoting psychological well-being alongside social harmony.
Insights from Family Therapy
Family therapy is a particularly suitable approach for working with the conflicts arising in a politically polarized group. The family therapist views the family as a system that is maintained and affected by each participating member. In politicized families, differentiation of self would be a core goal. The work would focus on allowing individuals to preserve their identity and beliefs while staying connected. No more “All liberals/conservatives are idiots” confrontations.
The primary goal of the therapist is to work collaboratively with family members to foster family unity despite political differences. Therapists can support clients in developing emotional resilience, asserting personal values, and engaging with family members from a stance of curiosity and respect rather than animosity.
In order to help family members improve their relationships, the therapist would focus on the following:
Reframing political arguments as representations of unmet emotional needs
Identifying and interrupting dysfunctional cycles of blame and moral condemnation
Exploring family of origin influences and intergenerational patterns
Setting boundaries around political discourse and promoting mutual respect
Practical Tools for Clinicians
The insights into working with polarized relationships gained from Family Therapy are generally useful for clinicians. In all family relationships, Safer (2019) emphasizes prioritizing love over politics and avoiding attempts to convert each other. People who believe that “I love my family member more than I love my politics” can more easily maintain a respectful relationship. The following are some basic guidelines and goals:
Couples: Encourage open and respectful conversations about political beliefs and teach skills such as reflective listening and emotional regulation.
Parents and Children: Help family members express appreciation for shared connections and respect each other’s unique perspectives regarding political dissimilarity.
Siblings: Help siblings reconnect with positive memories and enduring qualities of family identity beyond politics.
The Extended Family: Help politically divided family members abandon angry rhetoric or moral condemnation and reconnect to the shared history and importance of family relationships.
And finally, therapists should be prepared to teach and model skills that foster constructive dialogue and reduce defensiveness. These include:
reflective listening and emotionally focused communication;
boundary-setting strategies to limit exposure to partisan media or conversations; and
practicing dialectical thinking to better understand different world views.
Conclusion
Political polarization in families is on the rise. This increase is a relatively recent phenomenon, and therapists need to be equipped to help clients navigate this difficult terrain in a healthy way. A particularly helpful source of knowledge and strategies is Family Therapy, an approach that can help clients understand that the bonds they share are stronger and more enduring than any ideological divide. All clinicians, no matter what their modality, can adapt these tools for their own practices, helping to heal the broader social fabric, one family at a time.
Resources
An example of therapy with a politically divided couple is available on YouTube: “Helping Loved Ones Divided by Politics” with Dr. Bill Doherty
This article is adapted by the essay authors, L. Chamberlain & W. McCown from a chapter in their book, Psychotherapy in the Age of Political Polarization published in 2025 by Routledge. All quotes are from the authors’ or colleagues’ clinical experiences.
References
American Psychological Association (2024, December 10). After a divisive election, most U.S. adults ready to avoid politics this holiday. https://www.apa.org/news/press/releases/2024/12/avoid-politics-holiday
McCown, W., & Chamberlain, L. (2025). Psychotherapy in the age of political polarization: A guide for mental health professionals. Routledge.
Pew Research Center (2024, April 9). Partisanship by gender, sexual orientation, marital and parental status. https://www.pewresearch.org/politics/2024/04/09/partisanship-by-gender-sexual-orientation-marital-and-parental-status/
Safer, J. (2019). I love you, but I hate your politics: How to protect your intimate relationships in a poisonous partisan world. Biteback Publishing.
Yale University (Spring 2025). Yale youth poll. https://youthpoll.yale.edu/spring-2025-results
Biases Against Men in Couples Therapy
By Nafees Alam, PhD
When a couple begins therapy, both individuals should expect that their voices will be heard equally and their relationship dynamics examined with fairness and insight. However, for many men, the experience of couples therapy has become an unexpected tribunal where their masculinity itself stands accused. A negative view of men, which increasingly characterizes the broader culture (Alam, 2025a), is now evident in the clinical space (Alam, 2025b) threatening to undermine relationship healing processes.
This essay examines how biases against men manifest in couples therapy through stereotyping, blaming, ignoring, or misunderstanding male experiences. It explores the origins of these biases, their implications for men and society, and how therapists can work to correct these deeply unhelpful prejudices.
Background
Couples therapy emerged when gender roles were rigidly defined. Early models reinforced these structures, positioning women as emotional nurturers and men as rational providers. Feminist critiques in the 1970s and 1980s rightfully challenged these limiting paradigms, and therapeutic practice evolved to recognize the harmful effects of restrictive gender expectations.
However, this necessary correction has been overcorrected in some contexts. The term “toxic masculinity” exemplifies this problem, as the phrase inherently casts hostility toward the entire group it modifies. While women can engage in harmful stereotypically feminine behaviors, we don’t use “toxic femininity” because it’s obviously derogatory toward women as a whole. This linguistic double standard reveals a deeper bias where masculinity itself is increasingly treated as pathology rather than a complex gender expression containing both constructive and potentially destructive elements.
The American Psychological Association’s Guidelines for Psychological Practice with Boys and Men (2018) acknowledge the need for gender-sensitive approaches, yet implementation often falls short. Research by Seager et al. (2014) found that therapists are more likely to pathologize identical behavior when exhibited by male clients than female clients, suggesting systematic interpretive bias rather than individualized assessment.
How These Issues Play Out in Mental Health Treatment
In the therapeutic setting, biases against men manifest in several key ways:
Pathologizing typical masculine traits while failing to validate positive ones (Englar-Carlson and Kiselica, 2013). When men express emotions through action rather than words, this may be labeled as “emotional avoidance” rather than recognized as a different but equally valid emotional style. Masculine tendencies toward problem-solving are often framed as “avoiding intimacy” rather than legitimate approaches to connection.
Employing double standards in intervention (Alam, 2025a). When a woman withdraws from conflict, it may be interpreted as self-protection; when a man does the same, it is often labeled stonewalling. When a woman raises her voice, it might be seen as an appropriate assertion; when a man does so, it is frequently pathologized as aggression or intimidation.
Unconsciously assigning men the role of perpetrator and women the role of victim before understanding unique relationship dynamics (Alam, 2025a). This prejudgment appears in subtle ways: directing more challenging questions to the male partner, offering more empathy and validation to the female partner, or interpreting ambiguous situations through a lens that assumes male misconduct.
Engaging in “medical gaslighting” (Sebring, 2021), where men’s lived experiences are systematically invalidated. The man who insists his silence stems from feeling overwhelmed rather than a desire to control may be told he is “not being honest about his intentions.” The man who points out double standards may be accused of defensiveness rather than legitimate advocacy for fair treatment.
Possible Solutions
Anti-male bias in couples therapy does not work for men or women. Some possible solutions to correcting this contemporary bias include:
Develop training that explicitly addresses potential anti-male biases alongside other forms of prejudice. Therapists must recognize that masculine emotional expression may look different than feminine expression without being inherently deficient. Training should include case studies demonstrating how identical behaviors can be interpreted differently based on gender.
Develop and utilize assessment tools that account for diverse communication styles. Rather than expecting men to conform to feminine-typical modes of emotional processing, create validated instruments that recognize multiple paths to connection and healing, including activity-based interventions and solution-focused approaches.
Establish clear protocols for balanced intervention that ensure equal therapeutic attention and challenge to both partners. This includes structured approaches to questioning, validation, and confrontation that prevent unconscious gender bias from directing therapeutic focus.
Create male-friendly therapeutic environments by incorporating elements that research shows improve male engagement: clear structure, goal-oriented frameworks, and recognition of strength-based masculine traits alongside areas for growth.
Integrate routine bias checks into supervision and peer consultation. Regular case reviews should specifically examine whether gender biases are influencing case conceptualization and intervention choices.
Conclusion
Creating truly gender-inclusive therapeutic spaces requires courage from clinicians to examine their own biases, creativity to develop more flexible therapeutic approaches, and commitment to seeing each couple as unique individuals rather than representatives of their gender. It requires moving beyond simplistic narratives to recognize the complex reality that both men and women bring strengths and challenges to relationships (Capozzi, 2022).
By openly discussing and addressing biases against men in therapeutic spaces—just as we discuss biases against women—we create the possibility for more truly equitable treatment. The future of effective couples therapy lies not in taking sides in gender wars but in transcending them—creating spaces where both men and women can be seen, heard, and understood in all their complexity. Only then can therapy fulfill its promise of healing relationships rather than unconsciously reinforcing the divisions it aims to bridge.
References
Alam, N. (2025a, March 3). Why do so many men avoid mental healthcare? The urgent need for male-focused mental health campaigns and therapeutic approaches. Psychology Today. https://www.psychologytoday.com/us/blog/pop-culture-mental-health/202503/why-do-so-many-men-avoid-mental-healthcare
Alam, N. (2025b, February 14). Man versus bear: Who is the safer companion in the wild? Psychology Today. https://www.psychologytoday.com/us/blog/pop-culture-mental-health/202502/man-v-bear-who-is-the-safer-companion-in-the-wild
Alam, N. (2025c, February 12). Treating men like women—why men struggle in a mental health system built for women. Psychology Today. https://www.psychologytoday.com/us/blog/pop-culture-mental-health/202502/treating-men-like-women
American Psychological Association, Boys and Men Guidelines Group. (2018). APA guidelines for psychological practice with boys and men. https://www.apa.org/about/policy/boys-men-practice-guidelines.pdf
Capozzi, F. (2022). A multi-level guide to work with male clients in couple and family therapy from a gender-critical perspective. Journal of Feminist Family Therapy, 34(1–2), 178–195. https://psycnet.apa.org/doi/10.1080/08952833.2022.2065766
Englar‐Carlson, M., & Kiselica, M. S. (2013). Affirming the strengths in men: A positive masculinity approach to assisting male clients. Journal of Counseling & Development, 91(4), 399–409. https://psycnet.apa.org/doi/10.1002/j.1556-6676.2013.00111.x
Seager, M., Sullivan, L., & Barry, J. (2014). Gender-related schemas and suicidality: Validation of the male and female traditional gender scripts questionnaires. New Male Studies, 3(3), 34–54. https://newmalestudies.com/OJS/index.php/nms/article/view/151/154
Sebring, J. C. (2021). Towards a sociological understanding of medical gaslighting in western health care. Sociology of Health & Illness, 43(9), 1951–1964. https://doi.org/10.1111/1467-9566.13367
Improving Mental Health Care for Police Officers
By Kristopher Kaliebe, MD
“Therapists are not your friend and really could care less about you as a person. Never ever talk to them. They are liberal scumbags, or they wouldn’t be in that career.”
This police officer’s overgeneralization recognizes that many therapists’ viewpoints are incompatible with a sympathetic and supportive view of the police. Recognizing this bias, this essay argues for the critical need to develop and implement effective strategies to remediate these negative views and promote effective mental health treatments for law enforcement officers.
Bias in the Mental Health Field Against Law Enforcement Officers
There appears to be widespread anti-police bias across the different professions involved in the mental health field, as the following examples would attest:
In 2022, the American Psychological Association formed a resolution on psychology’s role in “dismantling” racist policing (p. 1).
The Journal for the American Academy of Child and Adolescent Psychiatry has declared itself to be an “anti-racist journal,” asserting that “We could fill these pages with the names of the Black people murdered by police officers, a devastating toll of racism in the United States.”
Social work is being shaped by social policy academics who support defunding the police. They argue that the police are tools of “social control and White supremacy” and that social workers should cease to collaborate with these agents enforcing racial dominance.
It is important to note that police officers’ overly negative portrayal is also influenced by a larger societal context that has adopted a social justice narrative. Three simplistic ideas are popular in mental health organizations and academia:
Traditional power structures are mostly harmful to society.
Discrimination is the fundamental cause of all unequal outcomes.
Problems should be seen primarily through the lens of race or gender or other markers of identity.
Such anti-police rhetoric, which is now well established in mental health institutions, professional bodies, and therapy services, is likely to influence therapists to:
view police as agents of oppression rather than unique individuals;
conceive of law enforcement officers with simplistic, false narratives; and
have reduced empathy toward officers.
What does this mean for police officers themselves? It is likely that this entrenched hostile rhetoric could undermine police officers’ trust in mental health professionals and discourage the use of employee assistance programs.
Mental Health Needs of Law Enforcement Officers
The mental health community should have the perspective that every law enforcement officer is an individual, requiring a personalized approach reflecting their needs, stressors, and treatment goals.
Therapists working with officers should consider the stresses of police work: trauma exposures, shift work, organizational stress, and disturbed sleep cycles. Law enforcement officers often interact with people at their worst. Police are scrutinized by the media and public and are easily criticized on social media. There is a reputational asymmetry; citizens and journalists can (and do) attack the reputations of officers by portraying their actions as misconduct (see here and here).
Yet, officers have few opportunities to explain their perspectives, and exoneration often takes years and does not make headlines. Police may have good benefits and adequate salaries, but they are certainly not rich. Judging by the mass exodus and lack of new recruits, the job of a police officer has become less appealing than ever.
Police may witness terrible traumas, and their work leads to increased rates of emotional distress when compared to the public at large. Officers often suffer from compassion fatigue, emotional numbing, and cynicism (Jetelina et al., 2020).
Most officers handle traumatic events well, but some develop severe trauma reactions, such as posttraumatic stress disorder (Corthésy-Blondin et al., 2022) along with work stress-related mental health disorders, such as depression and anxiety. Shift work is also hard on families, and the public needs police around the clock, including holidays, meaning officers’ schedules often conflict with family routines and special gatherings.
Police officers require determination and toughness, values that are sometimes at odds with asking for help. Officers must determine if their symptoms will decline over time or if they would benefit from professional mental health care. Fortunately, the law enforcement community has made a laudable effort over time to erode the stigma that portrays those seeking mental health care as lazy or weak. Yet, due to the critical nature of law enforcement, police administrators have procedures to remove officers that may be a risk to themselves or the public. As such, officers may worry that seeking help may signal an inability to handle their job and thus risk their removal from active duty.
Promising Interventions to Improve Mental Health Care for Law Enforcement Officers
Given the particular needs of police officers seeking help, we can identify some potential helpful interventions. To start, innovative programs can combine technology with anonymous surveys to help find officers who are most likely to benefit and help them access services (Deng et al., 2024). Then, in the clinical setting, the following approaches could be helpful:
Motivational approaches should prioritize goal setting and barriers to change (Steinkopf et al., 2015).
Mentalization (the ability to notice, access, and reflect on mental states in oneself and others) is an important skill for police and may be both an important focus of training for interfacing with the public and an important focus in individual therapy (Drozek et al., 2021).
Group therapies, whether online or in person, show potential for destigmatizing mental health treatment, efficiently spreading treatment, and utilizing the benefits of the group process.
Cognitive behavior therapy approaches have been applied to police (Lees et al., 2019), as have solution-focused therapies (Pooley et al., 2021).
Police officers’ mix of physical and emotional stressors (Mumford et al., 2014) suggests that physical wellness programs are desirable to encourage healthy lifestyles and robust physical conditioning and reduce substance abuse.
Family and marriage counseling may be especially beneficial for those in law enforcement (Sharp et al., 2022).
Finally, none of the above approaches are likely to work if police officers do not trust their therapists. Police counseling referral networks need to create a supportive, collaborative, and confidential environment. It is important to ensure therapists are equipped to effectively collaborate with police officers. Therefore, specialized training programs and workshops should be developed to address the unique challenges and stressors faced by law enforcement personnel. This training should include:
a comprehensive understanding of police culture and experiences;
building skills in trauma-informed care, resilience-building techniques, and evidence-based approaches tailored for the police community;
contributions from approaches across a range of psychotherapy modalities;
incorporation of peer consultations or ride-alongs with current officers or training from former officers to provide therapists with practical insights into the experience of law enforcement; and
technological innovations to enhance engagement with programs to increase fitness and overall health.
Conclusions
Some mental health professionals promote negative views of police officers and morally elevate, promote, and apply police-hostile theories through aforementioned policy statements, training programs, and scholarly journals. Mental health professional organizations must condemn any anti-police rhetoric that is arising from within their own ranks. Therapists must exchange anti-therapeutic ideologies for intellectual humility, the open exchange of ideas, and a focus on helping individuals.
It’s tragic that, under the banner of mental health, ideology has been weaponized against the law enforcement community. To address this problem, mental health professionals and the organizations that represent them should espouse balanced, fact-based views toward law enforcement, including noting research that questions narratives about pervasive racism and acknowledging positive trends in policing and the criminal justice system (Fryer Jr., 2019; Lattimore, 2022; Mangual, 2022).
References
Corthésy-Blondin, L., Genest, C., Dargis, L., Bardon, C., & Mishara, B. L. (2022). Reducing the impacts of exposure to potentially traumatic events on the mental health of public safety personnel: A rapid systematic scoping review. Psychological Services, 19(S2), 80. http://dx.doi.org/10.1037/ser0000572
Deng, Y., Frey, J. J., Osteen, P. J., Mosby, A., Imboden, R., Ware, O. D., & Bazell, A. (2024). Engaging law enforcement employees in mental health help-seeking: Examining the utilization of interactive screening program and motivational interviewing techniques. Administration and Policy in Mental Health and Mental Health Services Research, 1–15. https://psycnet.apa.org/doi/10.1007/s10488-024-01384-0
Drozek, R. P., Bateman, A. W., Henry, J. T., Connery, H. S., Smith, G. W., & Tester, R. D. (2021). Single-session mentalization-based treatment group for law enforcement officers. International Journal of Group Psychotherapy, 71(3), 441–470. https://doi.org/10.1080/00207284.2021.1922083
Fryer Jr, R. G. (2019). An empirical analysis of racial differences in police use of force. Journal of Political Economy, 127(3), 1210–1261. https://doi.org/10.1086/701423
Jetelina, K. K., Molsberry, R. J., Gonzalez, J. R., Beauchamp, A. M., & Hall, T. (2020). Prevalence of mental illness and mental health care use among police officers. JAMA Network Open, 3(10), e2019658. http://dx.doi.org/10.1001/jamanetworkopen.2020.19658
Lattimore, P. K. (2022). Reflections on criminal justice reform: challenges and opportunities. American Journal of Criminal Justice, 47(6), 1071–1098. https://doi.org/10.1007/s12103-022-09713-5
Lees, T., Elliott, J. L., Gunning, S., Newton, P. J., Rai, T., & Lal, S. (2019). A systematic review of the current evidence regarding interventions for anxiety, PTSD, sleepiness and fatigue in the law enforcement workplace. Industrial Health, 57(6), 655–667. http://dx.doi.org/10.2486/indhealth.2018-0088
Mangual, R. A. (2022). Criminal (in) justice: What the push for decarceration and depolicing gets wrong and who it hurts most. Center Street.
Mumford, E. A., Taylor, B. G., & Kubu, B. (2014). Law enforcement officer safety and wellness. Police Quarterly, 18(2), 111–133. https://doi.org/10.1177/1098611114559037
Pooley, G., & Turns, B. (2021). Supporting those holding the thin blue line: Using solution-focused brief therapy for law enforcement families. Contemporary Family Therapy, 1–9. https://link.springer.com/article/10.1007/s10591-021-09575-9
Sharp, M. L., Solomon, N., Harrison, V., Gribble, R., Cramm, H., Pike, G., & Fear, N. T. (2022). The mental health and wellbeing of spouses, partners and children of emergency responders: A systematic review. PLOS ONE, Jun 15;17(6):e0269659. https://doi.org/10.1371/journal.pone.0269659
Steinkopf, B. L., Hakala, K. A., & Van Hasselt, V. B. (2015). Motivational interviewing: Improving the delivery of psychological services to law enforcement. Professional Psychology: Research and Practice, 46(5), 348. http://dx.doi.org/10.1037/pro0000042
Treating Patients Impacted by Anti-White Racial Aggression
By Jaco van Zyl, MA
Racial discrimination, bias, or aggression toward people of any race is unethical. These experiences can impact people’s lives, leave lasting wounds, and negatively impact mental health. However, one form of racial aggression is often overlooked: aggression directed against people for being white. Although many clinicians have reported observing this phenomenon in their patients, training and clinical services on this issue are almost entirely nonexistent.
Research
A search of existing papers on this topic in the most common psychology database, PsycInfo, yields alarmingly few search results, none of which are in prominent clinical psychology journals (see Table 1 below). While academic research has focused on the prevalence, effects, and interventions in discrimination based on race, gender, and sexual orientation of other identity groups, there is hardly any research available where the group in question is white.
TABLE 1
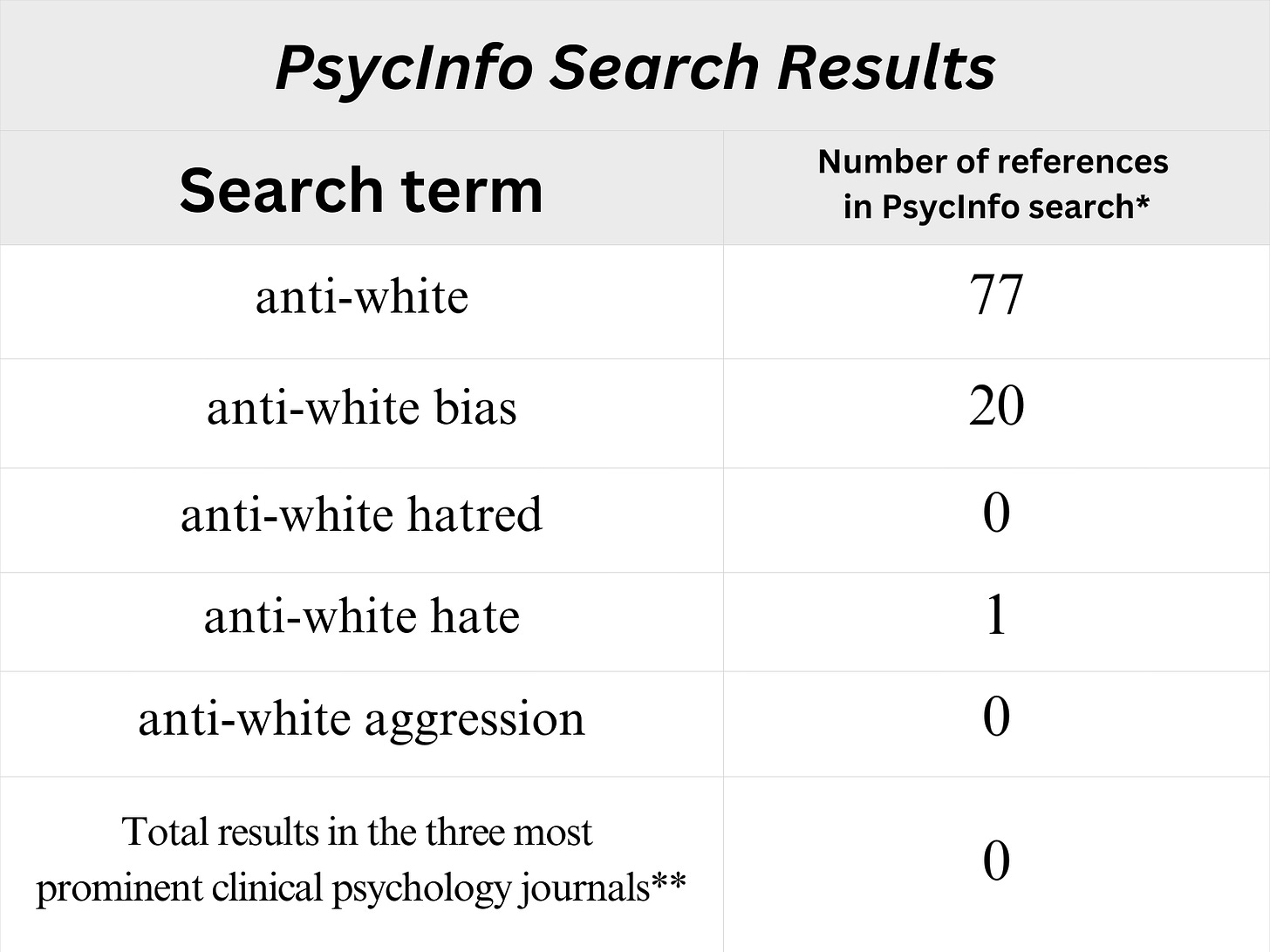
What we do find, however, are academic papers that advocate in favor of anti-white discrimination, diminish concerns about anti-white bias, and use language that is hostile or demeaning to white people. Some theories argue that white people are racist, ignorant, fragile, or privileged oppressors who need to be dismantled.
For example, one academic paper describes white racial identity as a “malignant, parasitic-like condition” without a “permanent cure.” Such “parasitic whiteness renders its hosts’ appetites voracious, insatiable, and perverse” (Moss, 2021, p. 355). Similarly, Noel Ignatiev (2002, p. 30) wrote that “the goal of abolishing the white race is on its face so desirable that some may find it hard to believe that it could incur any opposition other than from committed white supremacists.” Carter J. Carter (2023, p. 258) links “whiteness” to character pathology and even mass shootings. A widely circulated paper describes people with a white group identity as having “forms of pathological narcissism” (Miller & Josephs, 2013, p. 93). Another author (Edwards, 2016, para. 2) writes, “toxic whiteness keeps me bogged down in hesitation, fear, second-guessing, needs to get it right, and more.” These articles are full of language that communicates racial hostility and contempt.
Elsewhere, concerns about anti-white discrimination and its possible harm are framed as “whitelash.” This disregards these concerns as being fueled by a threat of status loss, and expressing these concerns is framed as a risk factor for delinquency (Isom Scott & Stevens Andersen, 2020). In most cases, this literature draws on a range of theories, such as critical race theory, decolonial theory, and whiteness studies, as theoretical lenses. Similar language and sentiments have made their way into every domain of civil society, including entertainment, news media, education, the corporate world, and politics.
Forms of Aggression and Bias
We can imagine how anti-white aggression and bias can take on many forms. At its most extreme, this may include recent crimes that were racially motivated and perpetrated against vulnerable working-class underage girls (Casey, 2025). Since exact numbers are unknown, estimates of 250,000 and 1 million victims have been called into question (Benedictus, 2025). In recent months, we have learned about the organized system of sexual assaults against underage girls in the U.K. and how violent physical and sexual assaults are motivated by anti-white hatred.
Other forms of anti-white bias and aggression include workplace and school bullying, verbal insults and harassment, hiring and selection discrimination, and training programs that deliberately or inadvertently humiliate participants for being white. Less obvious forms of anti-white bias may include neglect of the elderly, patients, children in foster care, and victims of crime. Some may also be aware of diversity, equity, and inclusion (DEI) initiatives in which white people—white males in particular—are being excluded from workplace hiring, promotion consideration, and training selection.
In February 2023, a group of black elementary school students in Ohio assaulted white students and ordered them to say, “Black Lives Matter” (Gentile, 2023). Likely, the vast majority of incidents like these never make the news. All this is to say that examples of the various types of anti-white aggression and bias are myriad.
Though empirical studies are missing, it’s clear that these incidents impact mental health. For instance, in July 2023, a highly respected principal in Toronto, Canada, took his own life after he was falsely accused of racism during a DEI training course in 2021 (Subramanya, 2023). Information about more cases like this is lacking because the topic seems to be systematically excluded from research.
As some may be aware, such anti-white sentiments and racially motivated discrimination have also reached the therapy room. Increasingly, clinicians and counselors report clients struggling with institutionalized discrimination and systemic indifference toward anti-white racism (Hartz, 2024).
Disappointingly, the standard instructions from British (here and here) and American regulatory bodies (here) have been to redirect and reframe the experience of targets and bystanders of anti-white injustice as “white fragility” (DiAngelo, 2018; Thomas, 2022). Targets of anti-white aggression and bias are often left disoriented and unsupported in a double-bind: If they accept attacks against them, they are guilty; but if they challenge them, they are even guiltier. Understandably, such anti-white bias has significant social and mental health implications.
Harmful Consequences
Depending on the form of anti-white aggression they experience, recipients of such action could:
develop clinical post-traumatic stress disorder from violent physical attacks perpetrated against them for being white,
experience shame and disorientation from experiencing unfair hostility and discrimination either directly or vicariously,
experience hypervigilance, chronic stress, depression, and anxiety from constant stigmatization at school, in the workplace, or the media,
resort to racial radicalization and violent retaliation in response to racialized abuse, or
engage in self-destructive behavior or attempt to appease attackers through self-denigration, imagining that allyship and self-hatred might appease their attackers.
Strikingly, none of these forms of anti-white racial aggression receives attention in mainstream civil society. Perhaps these experiences are dissociated, or people have been conditioned to accept them as normal. Yet for society at large, the normalization of anti-white aggression and bias could lead to significant problems, such as:
social fragmentation, eroding social cohesion and trust. Individuals in socially fragmented communities tend to be suspicious, withdrawn, and non-cooperative,
heightened risk of violence escalation and violent retaliation among fragmented communities,
perceptual blindness and reduced empathy for the suffering of vulnerable individuals, such as victims of crime, the injured, the infirm and elderly, patients, and children, and
younger generations potentially suffering from identity confusion and poor self-worth.
Remedies
Addressing anti-white aggression and bias requires a multifaceted approach. This may include:
research into the prevalence, effects, and treatment for anti-white aggression and bias,
policy changes to eliminate systemic discrimination arising from ideologies such as critical social justice,
clinical services (individual and group therapy) that are free from divisive ideology, where clinicians truly empathize with the experiences of affected individuals and populations,
public education that highlights the harm of race-based essentialism and demonization of all identities, white people included,
curriculum development and training for mental health professionals to adequately meet the needs of those who have experienced anti-white aggression and bias, and
protection and support for those who have experienced anti-white aggression and bias.
Conclusion
It can be painful, disorienting, and in some cases, tragic when people are the targets of bias and aggression based on race, gender, or sexual orientation. When these experiences are ignored, bias and aggression can become normalized. Popular discourse and anecdotal evidence suggest that there has been a rise in the incidence of anti-white aggression and bias, as well as apathy and perceptual blindness toward victims of such abuse.
Clinical services for this population are of the utmost importance. These patients need knowledgeable, open, and empathic therapists, not those who will judge, attack, or invalidate them. Additionally, research is crucial in determining the extent and impact of such events. This would improve understanding of the mental health effects of these experiences, which is necessary for developing effective interventions and promoting recovery in individuals and societies affected by bias and aggression against white individuals and communities.
References
Benedictus, L. (2025, January 8). How many children have been the victims of grooming gangs in the UK? Full Fact. Retrieved June 25, 2025, from https://fullfact.org/crime/grooming-gang-victims-musk-pearson-champion/
Carter, C. J. (2023). Whiteness catalyzes character disorder and mass violence. Studies in Gender and Sexuality, 24(4), 258–270. https://doi.org/10.1080/15240657.2023.2274796
Casey, L. (2025, June). National audit on group-based child sexual exploitation and abuse. https://assets.publishing.service.gov.uk/media/685559d05225e4ed0bf3ce54/National_Audit_on_Group-based_Child_Sexual_Exploitation_and_Abuse.pdf
DiAngelo, R. (2018). White fragility: Why it’s so hard for white people to talk about racism. Penguin Books.
Edwards, K. (2016, November 1). Toxic whiteness, the swamp of sadness, and healing. Keith Edwards. Retrieved August 3, 2025 from https://keithedwards.com/2016/11/01/toxic-whiteness-the-swamp-of-sadness-and-healing/
Gentile, L. (2023, March 3). Black students attack white students, force them to say ‘Black Lives Matter.’ Washington Examiner. Retrieved December 23, 2024, from https://www.washingtonexaminer.com/news/455628/black-students-attack-white-students-force-them-to-say-black-lives-matter/
Hartz, A. (2024, May 24). Mental health’s blind spot. City Journal. Retrieved June 28, 2025, from https://www.city-journal.org/article/mental-healths-blind-spot-for-antiwhite-bias-and-aggression
Ignatiev, N. S. (2002, September – October). Abolish the white race. Harvard Magazine, 105(1), 30. Retrieved August 3, 2025, from https://web.archive.org/web/20160311032753/http://harvardmagazine.com/2002/09/abolish-the-white-race.html
Isom Scott, D. A., & Stevens Andersen, G. (2020). ‘Whitelash?’ status threat, anger, and white America: A general strain theory approach. Journal of Crime and Justice, 43(4), 414–432. https://doi.org/10.1177/15570851241274863
Miller, A. E., & Josephs, L. (2009). Whiteness as pathological narcissism. Contemporary Psychoanalysis, 45(1), 93–119. https://doi.org/10.1080/00107530.2009.10745989
Moss, D. (2021). On having Whiteness. Journal of the American Psychoanalytic Association, 69(2), 355–371. https://doi.org/10.1177/00030651211008507
Subramanya, R. (2023, August 14). The deadly consequences of cancel culture. Spiked. Retrieved December 23, 2024, from https://www.spiked-online.com/2023/08/14/the-deadly-consequences-of-cancel-culture/
Thomas, V. (2022, December 27). Inserting critical social justice praxis into mainstream therapy — The broaching tool. Critical Therapy Antidote. Retrieved December 23, 2024, from https://criticaltherapyantidote.org/2022/12/27/inserting-critical-social-justice-praxis-into-mainstream-therapy-the-broaching-tool/
How Therapists Often Fail Religious Clients
By Neil J. Kressel, PhD
Statistically speaking, the typical client who walks into a therapist’s office is likely to encounter a practitioner who assigns far less importance to religion than does the client. One survey found, for example, that only about one-quarter of cognitive and behavioral therapists professed a certain belief in God. Just under half of the clinician sample deemed themselves nonbelievers (Rosmarin et al., 2013). Another study found that 50% of academic psychologists considered themselves atheists, and an additional 11% were agnostic. In this survey, psychology professors emerged as the least religious of all academics studied.
Background
The United States public overwhelmingly values religion and believes in God. Only about 4% say they are atheists, and—although the past decade may have witnessed some slight declines in religiosity—for quite a while, about nine out of ten American adults reported a belief in God. Seventy-seven percent identify with some religious faith. In the United States, 76% report praying at least sometimes, and 55% pray daily. While Western Europeans are somewhat less religious than Americans, many from other parts of the world tend to view religion as even more central to their lives.
People in need of psychological assistance may stay home if they feel that they will be openly or secretly denigrated because of their religious beliefs. The therapist-client gap in religiosity does not necessarily lead to insensitivity, but clinicians and patients report various difficulties that can impede therapeutic progress, even when everyone is well-intentioned.
Pastoral counseling can, of course, meet the needs of religiously observant clients who seek therapy within the context of a particular religious tradition. But plenty of people who do not choose this path still want—and would benefit from—a therapist with religious literacy and knowledge about faith-based issues.
How Current Practices Impact Clients
Though therapists exist at all levels of religiosity and a growing number nowadays think of themselves as “spiritual but not religious,” many are uncomfortable discussing religious matters in therapy, and some—when they do consider organized religion—view it mainly as a source of dysfunction. This is partly a legacy from Freud, Ellis, and other founders of clinical psychology. In 1993, the prominent Yale clinician Seymour B. Sarason commented with some concern that, if a psychologist learned that a colleague was “... devoutly religious, or even ... [tended] in that direction,” most of the time they would “... look upon that person with puzzlement, often concluding that [the] psychologist [in question] had or has personal problems” (Sarason, 1993). However, the reluctance to deal with religious matters also stems from a reasonable unwillingness to cross the line between therapy and proselytization for one’s own religious or nonreligious views, whatever they may be.
Another issue concerns the inadequacy of clinical training in teaching practitioners to handle religious issues in therapy (Vieten et al., 2016). In one study, about a fifth of therapists admitted to never discussing religious matters at all in therapy (Rosmarin et al., 2013). Several studies document psychologists’ belief that religion and spirituality have not been adequately addressed in their clinical education, despite the imperative to incorporate such issues as part of the diversity agenda (Jafari, 2016).
Sometimes, religious knowledge is needed to address specific client conditions. Research suggests, for example, that schizophrenia is no more likely among the religious. However, religiosity may influence how the condition expresses itself, for instance, in the content of particular delusions and hallucinations. Similarly, therapists might need some background in religion to distinguish culturally sanctioned religious behavior from pathology (Loewenthal, 2007).
What Should Be Done?
Mainstream therapy should not become faith-based, but several recent works have argued that neglect of religious issues can negatively impact the therapeutic process and client outcomes (Pargament et al., 2013). For starters, if a therapist seems uncomfortable or unreceptive to discussion of religious matters, a client may not share problems and potential solutions steeped in religion because they fear a negative response. Thus, a central part of the client’s life and significant resources for improvement would be inaccessible to the therapist.
Thousands of studies conducted over the past three decades have explored the relationship between religion and health, encompassing both physical and mental aspects (Kressel, 2024). By now, it is clear that religious beliefs and practices are often intertwined—for better or worse—with psychological well-being. Most meta-analyses of this literature have concluded that, on balance, religious belief and affiliation are net positives. For example, the religiously affiliated seem to receive benefits in maintaining longevity, managing mental health, coping with severe illness, avoiding substance abuse, and staying on the right side of the law. Needless to say, there is plenty of room for debate about why these correlations occur and their generalizability.
Proponents of a greater integration of religion into therapy argue that the world’s religious traditions, both Eastern and Western, can, at least sometimes, be a source of insight and mental health. They suggest that religion can provide a positive outlook, hope for the future, a sense of control, a pathway to meaning, constructive role models, and an ability to integrate loss (Rosmarin & Koenig, 2020). No reasonable person would claim that religion always provides these benefits, and it is not hard to see how religion could be a destructive force for some clients. Regardless, the religious aspect of clients’ lives must very often be examined in therapy by therapists who are at least willing to bracket their own preconceptions about faith.
Most psychologists would benefit from greater cultural competency in religious matters and from a fairer, more open-minded and more research-based attitude toward the role that religion plays in clients’ lives. Recently, some psychologists have argued in favor of formalizing religious and spiritual competencies for psychologists. Vieten and her colleagues (Vieten & Lukoff, 2022) developed sixteen religious and spiritual competencies and evaluated their acceptability to a sample of practitioners. Applying these competencies to practice, a therapist needs to:
show “empathy, respect, and appreciation” for clients from diverse spiritual, religious or secular backgrounds;
understand how one’s own religious or nonreligious outlook might influence one’s clinical approach;
develop awareness of various kinds of experiences clients might have with religion;
acquire familiarity with scientific studies and the psychology of religion;
help clients explore spiritual and religious resources that might aid in managing life concerns;
ask about spiritual and religious matters when they take a client history; and
consult with, or refer to, more qualified individuals when needed.
The boundary between religious belief and health care may be growing more porous. Several scholars, for example, have proposed various models for integrating spiritual and religious matters more effectively into cognitive-behavioral and rational-emotive therapy (Tan, 2013). Future research and debate should address whether and how these projects should proceed.
Conclusion
Even if one accepts that religion can be a constructive force, there are reasonable arguments for keeping aspects of religion out of therapy. More generally, clinicians should reassess and better articulate just how porous the wall between religion and therapy should be—and there is no reason to insist on one solution or to require that one size fits all. Still, most psychologists would benefit from a better understanding of the centrality of religious belief and practice in the lives of many who seek their assistance.
References
Jafari, S. (2016). Religion and spirituality within counselling/clinical psychology training programmes: A systematic review. British Journal of Guidance & Counselling, 44(3), 257–267. https://doi.org/10.1080/03069885.2016.1153038
Kressel, N. J. (2024). The psychology of religion: A social force. Cambridge University Press.
Loewenthal, K. (2007). Religion, culture and mental health. Cambridge University Press.
Pargament, K. I., Mahoney, A., Shafranske, E. P., Exline, J. J., & Jones, J. W. (2013). From research to practice: Toward an applied psychology of religion and spirituality. In K. I. Pargament, A. Mahoney, & E. P. Shafranske (Eds.), APA handbook of psychology, religion, and spirituality: Volume 2 An applied psychology of religion and spirituality (pp. 3–22). American Psychological Association. https://doi.org/10.1037/14046-001
Rosmarin, D. H., Green, D., Pirutinsky, S., & McKay, D. (2013). Attitudes toward spirituality/religion among members of the Association for Behavioral and Cognitive Therapies. Professional Psychology: Research and Practice, 44(6), 424–433. https://doi.org/10.1037/a0035218
Rosmarin, D. H., & Koenig, H. G. (Eds.) (2020). Handbook of spirituality, religion, and mental health (2nd ed.). Academic Press.
Sarason, S.B. (1993). American psychology, and the needs for transcendence and community. American Journal of Community Psychology, 21(2), 185–202. https://doi.org/10.1007/BF00941621
Tan, S.-Y. (2013). Addressing religion and spirituality from a cognitive-behavioral perspective. In K. I. Pargament, A. Mahoney, & E. P. Shafranske (Eds.), APA handbook of psychology, religion, and spirituality: Volume 2 An applied psychology of religion and spirituality (pp. 169–188). American Psychological Association.
Vieten, C., & Lukoff, D. (2022). Spiritual and religious competencies in psychology. American Psychologist, 77(1), 26. https://doi.org/10.1037/amp0000821
Vieten, C., Scammell, S., Pierce, A., Pilato, R., Ammondson, I., Pargament, K. I., & Lukoff, D. (2016). Competencies for psychologists in the domains of religion and spirituality. Spirituality in Clinical Practice, 3(2), 92–114. https://doi.org/10.1037/scp0000078
Black Sheep and Double Binds: Treating Minorities with Heterodox Viewpoints
By Lawrence Ian Reed, PhD
In 2020, two students from New York University (NYU) authored a petition demanding that the university implement Black student housing on campus. During that time, a Black student of mine came to me expressing considerable internal conflict over signing the petition. Although he preferred the existing housing system, he was told by several peers that he would be harming the Black community if he didn’t sign. He was also told that he would come to prefer the segregated housing if and when it was implemented. Months later, the student told me that he had reluctantly signed the petition but was relieved when NYU didn’t agree to the arrangement.
As this example shows, members of minority groups clearly have diverse opinions on every topic. But there’s a reason people don’t hear them more often: Complex pressures keep people silent.
The Black Sheep Effect, Double Binds, and the Spiral of Silence
When minorities express heterodox views, they typically risk a special kind of opposition from others within their group. One example is the “Black Sheep Effect” (Marques et al., 1988). This theory states that in-group members judge fellow in-group members with divergent viewpoints more harshly than they judge out-group members with those same viewpoints. This effect has been demonstrated with viewpoints regarding politics, race, and national identity (e.g., see here for examples). The result is that the minority member is not only opposed but marginalized within their own group—a group on which they often depend for most of their social support.
However, if they stay silent, they can feel inauthentic and equally isolated. A 2017 survey found that 49% of African Americans and 65% of Latinos stated that the political climate prevents them from saying things they believe (compared to 64% of Whites) (Cato Institute, 2017). Rather than responding spontaneously, they often decide in advance when, where, and with whom to share their views. Unfortunately, they often choose none of the above. As one Black student told me, “I always tell myself that I’m going to choose my battles, but I end up never choosing any of them.”
At root, these individuals often feel a double bind between group loyalty and personal authenticity (Shapiro & Heilman, 2024). But inauthenticity can lead to unique feelings of loneliness. The student above continued, “It’s bad because I’m not able to be myself around people. That leaves me without anyone to connect to. And, if I ever hear people say that they actually like me, my initial response is ‘Yeah, well, you probably wouldn’t if you knew all of my unpopular opinions.’” It's not hard to see how this kind of self-invalidation can be damaging and contribute to depression, anxiety, or other problems.
The result is what social psychologists call the spiral of silence (Noelle-Neumann, 1974). Individuals holding unconventional viewpoints often remain silent for fear of being marginalized. This leads others to also feel isolated, allowing self-censorship to spread. In contrast, individuals holding orthodox viewpoints are more likely to voice their opinions without fear—creating the appearance of a false consensus.
These apparent false consensuses prevent others from accurately understanding the views of the group. This could contribute to stereotyping of the group or even intergroup conflict if people assume everyone in a particular group thinks the same way. Even people within a given minority group may think less critically if they believe there is only one acceptable view for them to hold (Van Bavel & Packer, 2021).
How Can Clinicians Help?
Avoid Models That Pathologize Viewpoints
Some popular models in psychology pathologize minorities with heterodox views. One example is racial identity development frameworks, first developed by Helms (1990) and commonly taught in professional counseling training courses. In these models, there is a hierarchy of views ranging from disagreement with social justice ideology (at the bottom) to full adherence and activism (at the top). Minority individuals with heterodox perspectives would be classified as people who have not developed awareness of their racial identity. In other words, their views put them at the bottom of the hierarchy and mark them as in need of reeducation. Therapists who adhere to models like this could easily harm patients, leading to ruptures in the therapeutic alliance, self-censorship, and mistrust of the profession more generally.
Attend to Individual, Group, and Universal Factors
Arredondo et al. (1996) outline multicultural counseling competencies that emphasize personal identity at individual, group, and universal levels, encouraging a balanced approach that honors uniqueness alongside shared experiences. All too often with minority clients, the group level is overemphasized, and the individual and universal levels are de-emphasized. This framing reduces the space for minority clients to express their full range of views, values, and experiences. It makes sense for all three domains to be incorporated into treatments.
Use Therapies That Foster Authentic Expression
Some therapies might benefit from integrating Acceptance and Commitment Therapy (ACT). In ACT, clients learn to defuse self-censoring thoughts and commit to value-driven actions such as authentic expression, even in high-risk social contexts. Emerging evidence suggests this approach reduces loneliness by fostering psychological flexibility, particularly when combined with online support groups that connect heterodox individuals across geographic boundaries (Hayes & Hofman, 2018).
Build Communication Skills
Clients who have been self-censoring need support and practice to begin to articulate heterodox viewpoints in constructive ways. Strong communication skills, which patients may lack, are often essential to this process. Practical resources for clinicians can be found in recent publications on supporting free speech in therapy (Carmichael, 2025).
Conclusion
Members of minority groups with heterodox views can face myriad challenges: double binds, being targeted as black sheep, and conflicts around authenticity and connection. Therapists who foster authentic expression, individuality, and effective communication can help these patients overcome these kinds of barriers, which lead to silence and dysfunction.
References
Arredondo, P., Toporek, R., Brown, S. P., Jones, J., Locke, D. C., Sanchez, J., & Stadler, H. (1996). Operationalization of the multicultural counseling competencies. Journal of Multicultural Counseling and Development, 24(1), 42–78. https://doi.org/10.1002/j.2161-1912.1996.tb00288.x
Carmichael, C. (2025). Can I say that? Why free speech matters and how to use it fearlessly. Skyhorse Publishing.
Cato Institute. (2017, August 15-23). Cato Institute 2017 free speech and tolerance survey. Cato Institute. https://www.cato.org/sites/cato.org/files/survey-reports/topline/cato-free-speech-tolerance-toplines.pdf
Hayes, S. C., & Hofmann, S. G. (Eds.). (2018). Process-based CBT: The science and core clinical competencies of cognitive behavioral therapy. New Harbinger Publications.
Helms, J. E. (1990). Black and White racial identity: Theory, research, and practice. Greenwood Press.
Marques, J. M., Yzerbyt, V. Y., & Leyens, J. P. (1988). The “Black Sheep Effect”: Extremity of judgments towards ingroup members as a function of group identification. European Journal of Social Psychology, 18(1), 1–16. https://doi.org/10.1002/ejsp.2420180102
Noelle-Neumann, E. (1974). The spiral of silence. A theory of public opinion. Journal of Communication, 24, 43–51. https://doi.org/10.1111/j.1460-2466.1974.tb00367.x
Shapiro, E., & Heilman, S. (2024). Intercultural therapy with ultra-Orthodox Jews in Israel. Frontiers in Psychology, 15. https://doi.org/10.3389/fpsyg.2024.1356242
Van Bavel, J. J., & Packer, D. J. (2021). The power of us: Harnessing our shared identities to improve performance, increase cooperation, and promote social harmony. Little, Brown Spark.
Why Therapy with Men Must Recognize Biological Sex Differences
By William C. Sanderson, PhD
The mental health field is becoming increasingly female. For example, more than three quarters of doctoral psychology students are women (Callahan et. al, 2018). As this trend continues to accelerate, female representation in the profession is likely to exceed 90% within the next several years. Are there reasons to be concerned if male patients are primarily being treated by female therapists? Possibly—but potential problems can be reduced if therapists acknowledge that sex differences can impact treatments.
These issues, however, will be far more difficult to address if the mental health professions remain wedded to the notion that all observable differences between male and female behavior are solely the result of culture, with no biological contribution. This paper aims to shed light on this blind spot by exploring its implications for clinical practice and recommending ways in which therapy can be adapted to better meet the specific needs of male clients.
Why Does the Mental Health Field Ignore Sex Differences?
In recent years, the American Psychological Association (APA) accreditation process has mandated diversity training as a necessary competency. This move was based on the idea that therapists did not reflect the cultural and racial diversity of the population seeking treatment and that it is crucial for practitioners to better understand clients from diverse backgrounds. However, given that the male–female ratio is the largest demographic disparity between therapists and patients, it raises the question of why men’s issues were ignored as an area of diversity training.
One persuasive explanation for this gap is that the field of clinical psychology minimizes the significance of evolutionary psychology (Sanderson, 2020), which provides an empirical view of human nature, including explanations for the nature and function of sex differences (cf. Buss, 2023; Miller, 2000). Instead, clinical psychology holds to the standard social sciences model of human behavior, especially the blank slate hypothesis (Pinker, 2002). The blank slate hypothesis is the idea that all behavior is learned through experience and largely determined by the cultural environment. From this viewpoint, all observed differences between males and females are seen as a product of cultural socialization.
While the APA’s Guidelines for Psychological Practice with Boys and Men (APA, 2018) might appear to reflect an understanding of male–female differences, it again errs by overestimating the cultural influence on masculinity. The guidelines also broadly denigrate the nature of traditional masculinity—marked by stoicism, competitiveness, dominance, and aggression—as harmful, without highlighting the potential upside of these traits (e.g., stoicism, competitiveness, self-reliance). This omission is presumably because these are not aligned with socio-political ideologies that currently dominate the field of psychology (Ferguson, 2023).
Why Should Therapists Care About Sex Differences?
Numerous problems can arise from ignoring sex differences, including misunderstanding or missing men’s issues, failing to address the pressures of masculinity that may underlie psychopathology, and negatively stereotyping male or masculine qualities.
This may lead some therapists to struggle to connect with male patients. As a result, some patients may not benefit from therapy, prematurely drop out, or simply avoid therapy altogether. Scaffidi et al. (2024) found that although men have increased their use of mental health services in Australia, therapy dropout rates remain high, most commonly due to a lack of connection with therapists.
Challenges of Masculinity and How to Resolve Them
While data on increasing male engagement in therapy is lacking, several clear recommendations are worth considering until a more substantial evidence base emerges. To provide practical guidance for female and male therapists seeking to enhance their competence when working with men, these recommendations focus on engaging with common masculine traits rather than trying to deconstruct or challenge masculinity itself. The following four issues are most commonly raised across the existing literature (Levant & Wong, 2017; Barry et al., 2019; Seidler et al., 2018; Scaffidi et al., 2024):
Emotional control: Men are likely to attempt to remain emotionally controlled and may be less inclined to identify or express both positive and negative feelings. This can result in them appearing detached in therapy, which is focused on exploring emotional reactions. Adaptation: Treatment is likely to be more effective if therapists frame the therapeutic process as a way to build control, skill, and mastery that increase success across all areas of life. This skills-focused approach can make emotional engagement feel empowering, rather than presenting therapy as simply “helping men engage their feelings,” which could feel condescending, pointless, or emasculating to many men.
Self-reliance: Men are more likely to aspire to be self-reliant and may therefore be more reluctant to ask for help. Psychotherapy inherently involves some degree of reliance on the therapist. This attachment or dependence can make men feel overly dependent, leading them to compensate by minimizing the therapist’s role in treatment, which may reduce the therapy’s effectiveness. Adaptation: Therapists can frame therapy as a collaborative, active, problem-solving process rather than positioning themselves as the sole expert who will identify the problem. Using terms such as consultation or mentorship (especially for younger patients) may also resonate with some men. Normalizing help-seeking as a strength—similar to consulting a lawyer or other professionals—rather than a deficiency is a useful reframing.
Toughness or avoidance of weakness: Men are more likely to downplay emotional pain or distress to demonstrate toughness and are therefore reluctant to show vulnerability. This often leads to avoidance of exploring and expressing vulnerable emotions such as fear or sadness. Adaptation: The therapist should identify the patient’s strengths and toughness across a variety of situations while also normalizing that giving and receiving help and guidance at different points in life is a universal experience used by all leaders and other successful people. Metaphors to discuss the costs of toughness can reduce avoidance (e.g., ignoring physical pain and continuing to engage in a physical task will cause more harm in the long run).
Emotions viewed as universal and useful: Some men may devalue emotional expression in general because they perceive this as feminine, weak, or unnecessary. This may be particularly enhanced around topics such as relationship distress or work concerns, if these are perceived as contexts that men are expected to master. This belief may be amplified in therapy with a female therapist because the patient may automatically associate the approach with femininity. Adaptation: Providing psychoeducation to normalize the universal human experiences of all emotions can lead to increased comfort discussing emotions in therapy. The therapist can note that emotions serve important evolutionary functions and can be a source of inspiration, motivation, insight, and connection to others. In short, emotions exist and influence us whether or not they are acknowledged, and therefore, it is better to acknowledge and deal with them directly, rather than let them have unintended effects (e.g., use of alcohol to mitigate feelings, which can create other problems versus therapy).
Conclusion
Clinical psychology is dominated by female practitioners and is wedded to a particular social constructionist view of sex differences. To offer effective psychotherapy to male clients, clinical psychologists must understand the specific nature of male psychology grounded in biological sex. Training in the psychology of men is uncommon in academic programs and continuing education offerings, apparently for ideological rather than empirical reasons. In the long run, this will lead to a significant disservice to men seeking psychotherapy, leaving them without a useful resource to address various psychological concerns.
References
American Psychological Association, Boys and Men Guidelines Group. (2018). APA guidelines for psychological practice with boys and men. http://www.apa.org/about/policy/psychological-practice-boys-men-guidelines.pdf
Barry, J. A., Kingerlee, R., Seager, M., & Sullivan, L. (Eds.). (2019). The Palgrave handbook of male psychology and mental health. Springer.
Buss, D. M. (Ed.). (2023). The Oxford handbook of human mating. Oxford University Press.
Callahan, J. L., Smotherman, J. M., Dziurzynski, K. E., Love, P. K., Kilmer, E. D., Niemann, Y. F., & Ruggero, C. J. (2018). Diversity in the professional psychology training-to-workforce pipeline: Results from doctoral psychology student population data. Training and Education in Professional Psychology, 12(4), 273–285. https://doi.org/10.1037/tep0000203
Ferguson, C. J. (2023). The American Psychological Association’s practice guidelines for men and boys: Are they hurting rather than helping male mental wellness? New Ideas in Psychology, 68, 1–8. https://psycnet.apa.org/doi/10.1016/j.newideapsych.2022.100984
Levant, R. F., & Wong, Y. J. (Eds.). (2017). The psychology of men and masculinities. American Psychological Association.
Miller, G. (2000). The mating mind: How sexual choice shaped the evolution of human nature. Doubleday & Co.
Pinker, S. (2002). The blank slate: The modern denial of human nature. Viking.
Sanderson, W. C. (2020, June 29) Clinical psychology needs an empirical view of human nature. Psychology Today. https://www.psychologytoday.com/us/blog/our-evolutionary-selves/202006/clinical-psychology-needs-empirical-view-human-nature
Scaffidi, J., Wilson, M. J., Seidler, Z. E., & O’Shea, M. (2024). Expectations versus reality: Psychology trainees’ experiences working with men. Counselling Psychology Quarterly, 38(2), 251–269. https://doi.org/10.1080/09515070.2024.2373474
Seidler, Z. E., Rice, S. M., Ogrodniczuk, J. S., Oliffe, J. L., & Dhillon, H. M. (2018). Engaging men in psychological treatment: A scoping review. American Journal of Men’s Health, 12(6), 1882–1900. https://doi.org/10.1177/1557988318792157
How Socio-Political Values Shape the Therapeutic Alliance
By Nina Silander, PsyD
We are well aware that the therapeutic relationship has a great bearing on the success or failure of psychotherapy, more so than any other relevant factor (Lambert & Barley, 2001). The mystery and intrigue of the therapeutic alliance have been captured in popular culture, portrayed comically and dramatically in media, from TV series such as Monk and Ally McBeal to movies such as Anger Management and Good Will Hunting. While it is not always apparent what theoretical orientation or therapeutic interventions are at play in these portrayals, the centrality of the therapeutic alliance is palpable.
Meanwhile, values are enduring features in people’s lives, unlike transient emotional states, fluctuating symptoms, and fickle whims (McMinn et al., 2016). Values, distinct from attitudes and interests, are “foundational commitments” upon which the latter two rest. They are frequently informed by spiritual, religious, and/or ideological worldviews, which posit answers to questions about the meaning of life and suffering, the nature of human relationships, and how we should live in the material world. Shy of these most existential questions, values that arise in therapy pertain to a wide range of issues, such as marriage and romantic relationships, parenthood decisions, career choices, spiritual and religious beliefs and practices, the use of social benefits, and civic engagement.
Values as Glue or Solvent
People are attentive to others’ attitudes, beliefs, and values, and clients and therapists are no different when navigating clinical services. Clients carefully select therapists from directories based on first impressions and according to personal recommendations; therapists consider client characteristics when accepting referrals and devising treatment plans. Additionally, establishing a therapeutic alliance during the early sessions is predictive of whether therapy will end prematurely (Smith, 2019). Understandably, people prefer others who share their values and are less comfortable with those who don’t (Brandt & Crawford, 2019). So, inconsistency in values can rupture the therapeutic alliance, while consistency in values strengthens it. This pattern is, of course, replicated in other areas of public life, such that people seek proximity to or affiliation with those who possess shared traits—whether demographic characteristics, sociopolitical values, religious beliefs, income level, lifestyle, or recreational interests.
Politics as a Source of Values Conflict
Unsurprisingly, the intensifying climate of political polarization is straining communities, as well as the therapeutic relationship in treatment. The adoption of virtually monolithic left-wing politics by mental health professional organizations and their members has resulted in a range of concerning downstream effects, including open hostility and willingness to discriminate against outgroups (i.e., those who are not firmly left-wing) (Inbar & Lammers, 2012). This development is shocking for professionals trained to self-reflect, value equality and fairness, and, in most other circumstances, be temperamentally open to new experiences and ideas—self-selection into these professions is, in part, due to such traits.
Suggestions for Managing Values in Therapy
Long-standing disagreements have existed regarding the feasibility of therapists adhering to value neutrality and objectivity—an aspiration set forth by Freud, who sat behind his clients to avoid distracting them during the articulation of their streams of consciousness. Values neutrality was reinforced during subsequent schools of psychology. Since then, many have questioned whether this degree of neutrality is possible or appropriate. Others believe that therapy is inherently “value-laden” because therapists cannot avoid drawing on their conceptions of human nature when guiding the therapeutic process and determining what is in a client’s best interest (e.g., Fisher-Smith, 1999). As such, therapists must exercise caution in determining how their values might manifest in psychotherapy (McMinn et al., 2016) or under what conditions therapist influence on clients’ values is acceptable. It is well-known that clients are readily influenced by therapists’ values (Tjeltveit, 1986).
Rather than practicing American Psychological Association Ethics Code recommendations (e.g., respect others’ cultural and spiritual backgrounds, guard against personal bias, and strive for impartiality), many left-wing therapists call for politicizing social justice in clinical practice and promoting critical consciousness among clients, irrespective of their personal therapy needs and goals (Barraclough et al., 2024). Yet, especially compared to the recent “therapist-activist” movement, an aspiration toward tempered and careful engagement with the values of psychotherapy is essential, out of concern for client autonomy and an appropriately constrained therapist role.
Several methods have been suggested for navigating values carefully in therapy. Jackson et al. (2013) propose numerous strategies that involve serious considerations. They include making decisions to:
distinguish between professional values (e.g., values about decreasing psychiatric symptoms during therapy) and personal values (e.g., sociopolitical values), which some believe to be a false dichotomy;
carefully disclose personal values, which could jeopardize the therapeutic relationship at the outset of treatment;
refer clients to other therapists who share similar values, though doing so could limit access to care (i.e., too few non-left-wing therapists to meet the population-level need);
adjust therapeutic goals, such that a therapist truncates their vision and professional values to prioritize a client’s personal values and autonomy; and/or
seek outside consultation to develop professional perspectives and skills.
Jackson et al. (2013) ultimately suggest that therapists need in-depth training to effectively “articulate their ontological and philosophical assumptions and show how they relate to their theory of change, interventions, and evidence of change” (p. 11). In this way, therapists can make their decisions clinically guided and client-relevant.
Another suggestion for mitigating the influence of inappropriate values has been the concept of time- and context-bound “value bracketing” and the integration of values (McWhorter, 2019). According to McWhorter’s (2019) model, therapists bracket personal values (“private values from values regulating professional work,” p. 210) during the clinical interviewing stage, before accounting for both therapists’ professional and personal values, as well as the client’s values, during the treatment planning stage. McWhorter (2019) suggests that this is appropriate as therapists would not “agree to pursue client proposed goals that are inconsistent with a client’s assessment results, diagnosis, customary evidence-based treatment practices, or professional legal obligations” (p. 216). While treatment goals would originate from the client, both therapist and client would ultimately assess and consent to them. This model simultaneously preserves client autonomy and protects therapists’ moral conscience.
Conclusion
Unlike the objective neutrality required for scientific research and much of psychological evaluation, navigating values in psychotherapy is an inescapable task that each therapist will encounter eventually and repeatedly. In an increasingly politically polarized cultural climate that persuades and pressures therapists to function as activists, therapists must consider how to professionally manage their personal values. Sociopolitical values, once arguably relegated to an entirely personal domain, must also be accounted for, especially for the sake of developing a robust therapeutic relationship—the linchpin of effective treatment.
References
Barraclough, S., Malott, K., & Ahuriri-Driscoll, A. (2024). Broaching client identities: Integrating a critical consciousness lens in counseling practice. International Journal for the Advancement of Counselling, 46, 149–170. https://doi.org/10.1007/s10447-023-09535-y
Brandt, M. J., & Crawford, J. T. (2019). Worldview conflict and prejudice. Advances in Experimental Social Psychology, 61, 1–66. https://doi.org/10.1016/bs.aesp.2019.09.002
Fisher-Smith, A. M. (1999). From value neutrality to value inescapability: A qualitative inquiry into values management in psychotherapy. (Unpublished doctoral dissertation). Department of Psychology, Brigham Young University, Provo, UT.
Inbar, Y., & Lammers, J. (2012). Political diversity in social and personality psychology. Perspectives on Psychological Science, 7(5), 496–503. https://doi.org/10.1177/1745691612448792
Jackson, A. P., Hansen, J., & Cook-Ly, J. M. (2013). Value conflicts in psychotherapy. Issues in Religion and Psychotherapy, 35(1), 6–15. Available at: https://scholarsarchive.byu.edu/irp/vol35/iss1/3
Lambert, M. J., & Barley, D. E. (2001). Research summary on the therapeutic relationship and psychotherapy outcome. Psychotherapy: Theory, Research, Practice, Training, 38(4), 357–361. https://doi.org/10.1037/0033-3204.38.4.357
McMinn, M., McLaughlin, P. T., Johnson, B. C., & Shoup, R. (2016). Psychotherapy and the theological virtues. Open Theology, 2(1), 424–435. https://doi.org/10.1515/opth-2016-0035
McWhorter, M. R. (2019). Balancing value bracketing with the integration of moral values in psychotherapy: Evaluation of a clinical practice from the perspective of Catholic moral theology. The Linacre Quarterly, 86(2–3), 207–224. https://doi.org/10.1177/0024363919856810
Smith, A. M. (2019). The relationship between therapeutic alliance and client progress in predicting premature termination in counseling. (Publication No. 29238401) [Doctoral dissertation, Texas A&M University]. ProQuest Dissertations & Theses Global.
Tjeltveit, A. C. (1986). The ethics of value conversion in psychotherapy: Appropriate and inappropriate therapist influence on client values. Clinical Psychology Review, 6, 515–537. https://doi.org/10.1016/0272-7358(86)90035-8
Cultural Misunderstandings: On the Misuses of the Term “Culture”
By Douglas Novotny, PhD
Over the past decades, the mental health field has been taken over by the concept of “cultural competency.” This term sounds like it could refer to the myriad dynamics of culture that shape people’s lives, but in practice, it’s typically code for left-leaning identity politics (particularly race, gender, and sexual orientation). This is a huge loss. When culture is reduced to race or other demographic categories, it blinds us to real human diversity and the complex processes that shape our lives.
Static Trait vs. Dynamic System
Two contrasting models of culture illustrate how each leads to very different understandings—culture as a trait and culture as a dynamic system:
Culture as a trait (e.g., race). This view dominates much of the academic discourse today. Material indicators of culture (i.e., demographic categories) render it a static and concrete trait. This model is shallow and partial in that so much of culture is left out. It can encourage labeling oneself or others in ways that deny human complexity.
Culture as a dynamic system. This view adds depth and complexity. Cultural systems carry knowledge, practices, and values through generations. Culture here is closer to a story than a label. Broader and deeper than any person or trait, it’s the context within which we live. And it extends beyond racial categories, so it could include things such as American culture or Catholic culture (Baldwin et al., 2006; Frisby, 2018; Redding & Cobb, 2023; Shweder, 1991, 1993).
Given that the dynamic system model has so much more depth and accuracy in defining culture, why is the trait model ascendent? It could be that the trait model is appealing precisely because it’s oversimplified and concretized. Society is in flux, and complex models are harder to understand. The trait model could reduce anxiety and distress about this flux and complexity, making culture feel more knowable and controllable—even as it hollows the concept of its richness.
This reductionism resembles the psychoanalytic concept of a “fetish.” Here, fetish doesn’t refer to “kink” but to a fixation, a maladaptive focus on concretized manifestations of desire. Consider the classic example of a foot fetish. Attraction for a whole person collapses into desire for a part-thing, such as a foot. Similarly, today’s trait-model of culture preoccupies itself with part-things such as skin tone or genitals—things that aren't culture at all, but appearances that are at most partial representations of it. Fetishizing superficial traits can reduce distress and uncertainty, but doing so can erase our humanity.
The Psychosocial Toll
The trait model of culture can cause a number of problems, such as:
It’s reductionistic. Forcing people into procrustean beds of trait labels or body parts blinds us to internal nuance and paradoxical aspects of character. Therapists are now trained to impose racialized categories, even for clients who don’t view themselves or their problems that way. Tying people too strongly to these categories can prevent them from accessing individuality and depth, reduce them to superficial traits, or deny them free will.
It derails human connection. The trait model prominently uses labels such as “Asian” to categorize people, but this can redirect away from genuine human connection. For example, this model grossly oversimplifies the enormous variation in cultures and histories among—and including conflict between—societies in Asia. The label “Asian” equates a young, urban, secular, Marxist Korean woman with an elderly, religious, rural Japanese CEO man, overlooking vital aspects of culture and character that are as important, if not more important, than a shared connection to the Asian landmass.
It impoverishes language. Trait identity labels often oversimplify, confuse, or demean more than they describe or comprehend. For instance, the acronym LGBTQIA lumps together several groups (Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, and Asexual), but it isn’t clear how same-sex attraction (body intact and comfortable) increases comprehension of or affiliation with someone’s gender dysphoria. Thus, the fixed categorical structure of traits is poor. By contrast, dynamic systems are rich and played out in stories where character development and nuance can be fleshed out.
It divides. When identity traits define cultural categories, people get equated with those categories and traits. But this identity politics fuses the thought with the thinker. Instead of a person with an idea to consider, one becomes a mere avatar or representative of group membership, purportedly representing the group as a block. Today, people often begin statements as follows: “speaking as a … [fill-in-group-identity-trait-here].” This conflation of thought and thinker undermines efforts to disagree civilly, because once my idea is fused with my identity, then any attack on my idea feels like an attack on me or my very existence. Thus, the trait model casts group against group, and identity politics culture wars become ever-present and intractable.
Escaping the Culture Confusion Trap
True culture is fascinating and evocative, like a novel, the arts, or cinema. A person, an education, or the arc of therapy can be fruitfully understood in this way. By contrast, fetishized culture diminishes anything or anyone viewed through that lens. No one should be regarded as a mere set of concrete traits, least of all by professionals whose job it is to see beyond—and not be bound within—dehumanizing tendencies.
The recognition of culture as a dynamic system helps therapy in the following ways:
True diversity. Therapists mindful of dynamic cultural systems can more effectively embrace diversity: varied perspectives, intergenerational values, mythic tales, spiritual accounts, art and architecture, families, and other social bonds.
Bridging ideological pitfalls. A focus on controversies such as policing and race can impair treatment if a hot topic detracts from psychological awareness or if there is a perceived incompatibility between the client and the therapist. Such topics are often seen exclusively through a trait-culture lens (e.g., presuming trait discrimination is the one and only explanation for bad events). Therapists can more fully comprehend ideological preoccupations and navigate disagreements by familiarizing themselves with cultural accounts (e.g., Hughes, 2018; Riley, 2015) that acknowledge discrimination while moving beyond superficial trait-level thinking.
Depth of experience. The trait model emphasizes competitive group status (e.g., “privilege”), whereas deeper comprehension is invited in the dynamic system model. A therapist’s duty is to help improve one’s meaningfulness in life, whatever one’s group or status is. Grief stings no less—sometimes more—if one has had good luck in other ways. And the delights of life should be honored, even—especially, perhaps—among those who’ve had too few of them.
Clinical utility. Culturally rich concepts such as “disgust” and “soul” have immense therapeutic value. For example, they can predict suicidality (Rottman et al., 2013). Therapists aware of true culture can more readily explore the concepts of disgust and soul with the many patients who would benefit from a deeper understanding of them. Superficial cultural trait labels lack such depth.
None of this suggests that trait-related cultural labels should be dismissed out of hand. When traits embody deep, enduring meanings, those should be honored. The point instead is that therapists should look for deeper resonances rather than accepting superficial labels or identities as the sole determinant of a client’s cultural experience.
Conclusion
Our society is now gripped by a harmful fixation. It mistakenly views culture as a set of traits rather than the dynamic system it properly is. Thus, psychology has fallen into an identity-politics trap that concretizes and demeans people instead of elevating them and engaging in their complexities. By shifting toward a more dynamic and accurate view of culture, we can avoid these traps, improve mental health care, and help people access their uniqueness, humanity, and depth.
References
Baldwin, J. R., Faulkner, S. L., & Hecht, M. L. (2006). A moving target: The illusive definition of culture. In J. R. Baldwin, S. L. Faulkner, M. L. Hecht, & S. L. Lindsley (Eds.), Redefining culture: Perspectives across the disciplines (pp. 3–26). Routledge.
Dogruyol, B., Alper, S., & Yilmaz, O. (2019). The five-factor model of the moral foundations theory is stable across WEIRD and non-WEIRD cultures. Personality and Individual Differences, 151(1). https://doi.org/10.1016/j.paid.2019.109547
Frisby, C. L. (2018). Viewpoint bias and cultural competency advocacy within applied psychology. In C. L. Frisby & W.T. O’Donohue (Eds.), Cultural competencies in applied psychology (pp. 169–207). Springer.
Hughes, C. (2018, May 14). The racism treadmill. Quillette. https://quillette.com/2018/05/14/the-racism-treadmill/
Paresky, P. (2019, December 21)). The tribal morality of identity politics. American Mind. https://americanmind.org/features/you-gotta-serve-somebody/the-tribal-morality-of-identity-politics/
Redding, R. E., & Cobb, C. (2023). Sociopolitical values as the deep culture in culturally-competent psychotherapy. Clinical Psychological Science, 11(4), 1–17. https://doi.org/10.1177/21677026221126688
Riley, J. (2015). Race relations and law enforcement. Imprimis, 44(1). https://imprimis.hillsdale.edu/race-relations-and-law-enforcement/
Rottman, J., Kelemen, D., & Young, L. (2013). Tainting the soul: Purity concerns predict moral judgments about suicide. Cognition, 130, 217–226. https://doi.org/10.1016/j.cognition.2013.11.007
Shweder, R. (1991). Thinking through cultures: Expeditions in cultural psychology. Harvard University Press.
Shweder, R. (1993). “Why do men barbecue?” and other postmodern ironies of growing up in the decade of ethnicity. Daedalus, 122(1), 279–308. https://www.jstor.org/stable/20027159
Codifying Bias: How Activist Politics Became Embedded in Social Work Standards and Practices
By Nafees Alam, PhD
Social work, a profession dedicated to helping vulnerable populations, has increasingly embraced a narrow ideological framework that threatens its core mission. The phrase “I’m a social worker; what’s your superpower?” reveals a troubling hero complex emerging within the field, in which practitioners position themselves as saviors rather than facilitators of client autonomy. What is even more concerning is the way the profession has shifted from client-centered care to the advocacy of predetermined political positions under the guise of social justice.
In this essay, I will consider how this shift has come about, what it means for professional practice, and how practitioners can offer helpful solutions to restore balance to the profession.
Background
Social work emerged in the late 19th century with dual roots: charity organization societies focused on individual assistance and settlement houses addressed community needs. While clinical interventions and community organization represent different approaches, both are traditionally centered on “meeting the individual where they are” and understanding each client’s unique circumstances and needs (Raine et al., 2023).
Since its inception, social work has been oriented toward progressive causes, with pioneers such as Jane Addams advocating for social reform. This progressive orientation, however, was historically balanced with rigorous clinical training and respect for client self-determination. Today, this balance has shifted dramatically toward enforced ideological conformity, and professional bureaucratic structures have facilitated this.
The following examples illustrate how professional organizations use ideologically loaded concepts to pressure practitioners into incorporating political ideologies into their work—often in ways that impinge on the equal treatment of clients, client autonomy, and respect for the diversity of clients’ values:
The 2022 Council on Social Work Education (CSWE) accreditation standards require curricula to be focused on “dismantling systems of oppression” (p.16). For example, Standard 3.1 mandates that programs must “engage diversity in their practice” with explicit instruction on anti-racism and guidance on “how mechanisms of oppression and discrimination” impact well-being.
Some social work journals now prioritize anti-oppressive perspectives over methodological rigor. For instance, the Journal of Progressive Human Services explicitly states in its aims and scope that it is “covers political, social, personal, and professional problems in human services from radical and anti-oppressive perspectives” and “assumes that the economic, political, social, and cultural structures privilege some and not others,” rather than emphasizing empirical standards first.
The National Association of Social Workers (NASW) Code of Ethics mandates “social and political action” (p.1) as an ethical obligation. Section 6.04 specifically requires social workers to “engage in social and political action that seeks to ensure that all people have equal access to the resources, employment, services, and opportunities they require to meet their basic human needs and to develop fully” (p.8).
Educational programs increasingly evaluate students on ideological conformity rather than clinical skills. For example, Holmström (2013) documented how social work programs “assess and develop moral character” (p. 451) in social work education.
How These Issues Play Out in Mental Health Treatment
The consequences of this ideological shift are particularly evident in mental health settings (Farber & Fram, 2024). Consider the following examples:
Practitioners face professional pressure to view religious clients through an oppression lens rather than respecting their belief systems, as documented in Hodge’s (2020) study on religious discrimination in social work. In practice, this often manifests as encouraging clients to critically examine their religious beliefs as potential sources of internalized oppression rather than working within their faith framework when providing therapeutic services.
Social workers who question aspects of gender-affirming care report professional ostracism, as revealed in Lindroth et al.’s 2025 study. Clinicians who raise concerns about the rapid increase in adolescents identifying as transgender or who suggest exploratory therapy before medical interventions often face accusations of transphobia and exclusion from professional networks.
Clinicians report being unable to discuss certain therapeutic approaches that are deemed problematic, limiting evidence-based practice options, as shown in Duarte et al.’s 2015 research. For example, cognitive-behavioral approaches that focus on personal agency and responsibility are sometimes criticized as blaming the victim or ignoring systemic factors, despite their proven efficacy for many conditions.
Faculty members expressing viewpoint diversity concerns face hostile work environments, as documented in multiple academic freedom cases. The case of Mark Regnerus at the University of Texas and similar instances show how scholars questioning orthodoxy face professional retaliation, including calls for termination.
This enforced orthodoxy prevents honest clinical discussion about complex cases and has a chilling effect on evidence-based practice. It undermines the profession’s ability to serve diverse clients and creates situations in which clients with traditional or conservative views may receive biased care or are made to feel that their perspectives are pathologized rather than understood.
What Can Be Done?
The social work profession is facing problems of immense scale, and the issues are all interrelated and multidimensional. The solutions are simple, but an important starting point would be to offer a clearer field-wide analysis to inform an effective corrective turn. To this end, there are at least four domains requiring immediate action.
Educational Reform
Educational reform must be central to this effort, focusing on restoring intellectual diversity to social work programs:
Curriculum balance: Implement reading lists that include diverse ideological perspectives and challenge orthodoxy. The Heterodox Academy’s Teaching & Advocacy Resources offers practical approaches, such as viewpoint diversity audits of syllabi and frameworks for facilitating discussions on controversial topics.
Protected classroom discourse: Create environments in which students can debate controversial issues without fear of academic penalties, following the University of Chicago’s Principles of Free Expression. This includes explicit protections for students expressing unpopular views during class discussions and in written assignments.
Diverse faculty recruitment: Develop hiring practices that value intellectual diversity and different theoretical orientations, not just demographic representation. This might include adding “commitment to viewpoint diversity” as a criterion in faculty searches and ensuring that hiring committees themselves represent diverse perspectives.
Professional Organization Reform
Organizations such as the NASW and CSWE need significant reforms to restore professional neutrality:
Revise ethical standards: Return the code of ethics to its client-centered focus rather than prescribing specific political activism. This would involve modifying Section 6.04 to emphasize that social workers should advocate for policies that benefit clients without mandating particular political positions.
Outcome-based accreditation: Shift accreditation standards toward measuring clinical competencies and client outcomes rather than ideological compliance. This would prioritize demonstrating effectiveness in improving client well-being over adherence to particular theoretical frameworks.
Member advocacy: Support the formation of interest groups within professional organizations that advocate viewpoint diversity and intellectual freedom. The recently formed ProSocial Workers represents one such effort to create space for professional dissent.
Research Standards Reform
The research ecosystem in social work requires structured interventions:
Methodological focus: Journal editorial boards should prioritize research rigor over ideological alignment with transparent peer review processes. This includes encouraging pre-registration of studies and embracing methodological pluralism rather than privileging particular epistemological approaches.
Diverse research questions: Funding bodies should support investigations across the ideological spectrum on controversial topics. This would include studies examining potential negative outcomes of interventions that are currently considered best practices based on ideological rather than empirical grounds.
Replication emphasis: The field should prioritize replication studies to test whether ideologically aligned findings hold up to scrutiny. Organizations such as the Center for Open Science offer frameworks to improve reproducibility and transparency in social science research.
Professional Dissent Networks
Building supportive networks for practitioners with diverse viewpoints is essential:
Practitioner communities: Support emerging groups such as Heterodox Social Work that provide safe spaces for professional discussion. These communities allow clinicians to share experiences, discuss complex cases, and develop practice approaches outside ideological constraints.
Legal protection: Connect practitioners facing viewpoint discrimination with legal resources through organizations such as the Foundation for Individual Rights and Expression. This provides a safety net for clinicians who face professional retaliation for expressing heterodox views.
Client advocacy: Develop resources for clients seeking ideologically diverse practitioners who will respect their values and beliefs. This might include directories of practitioners committed to client-centered rather than politically driven approaches to therapy.
Conclusion
Social work stands at a crossroads. The profession can continue down the path of ideological conformity, potentially alienating clients and practitioners with diverse viewpoints, or reclaim its rich tradition of client-centered care within ethical boundaries that respect intellectual diversity (Farber, 2023). It’s not an overstatement to suggest that ongoing politicization of the field could lead to broad cuts in government funding and other legislative changes that could gut the profession.
The general public deserves to understand what social work is and what it could be. Rather than a profession defined by political activism, social work at its best combines compassion with evidence-based interventions tailored to individual needs. It respects client autonomy while providing expert guidance and addresses systemic barriers without imposing predetermined political solutions.
As scholars and practitioners increasingly challenge ideological capture, there is hope that social work can evolve toward taking a more balanced approach that upholds the profession’s core values while embracing intellectual diversity (Alam & Rueda, 2025). The profession is beginning to challenge ideological capture. Recently, one social work journal (The Journal for Teaching in Social Work) published a special issue on critiquing ideological mandates in the profession, and it is currently calling for papers on academic freedom and critical thinking in social work. This evolution would benefit social workers and the diverse populations they serve, ensuring that all clients receive care that respects their unique circumstances, beliefs, and aspirations.
References
Alam, N., & Rueda, H. (2025). Heterodox social work: Advancing viewpoint diversity, constructive disagreement, and open inquiry. Research on Social Work Practice, 0(0). https://doi.org/10.1177/10497315251351865
Council on Social Work Education. (2022). Educational policy and accreditation standards. CSWE. https://www.cswe.org/accreditation/policies-process/2022epas/
Duarte, J. L., Crawford, J. T., Stern, C., Haidt, J., Jussim, L., & Tetlock, P. E. (2015). Political diversity will improve social psychological science. Behavioral and Brain Sciences, 38, e130. http://dx.doi.org/10.1017/S0140525X14000430
Farber, N. (2023). The dystopian world of social work education. Academic Questions, 36(4), 17–25. https://doi.org/10.51845/36.4.5
Farber, N. B., & Fram, M. S. (2024). The danger of ideology: Social work, Israel, and anti-Semitism. Social Work, 69(2), 204–206. http://dx.doi.org/10.1093/sw/swad052
Hodge, D. R. (2020). Spiritual microaggressions: Understanding the subtle messages that foster religious discrimination. Journal of Ethnic & Cultural Diversity in Social Work, 29(6), 473–489. https://doi.org/10.1080/15313204.2018.1555501
Holmström, C. (2013). Suitability for professional practice: Assessing and developing moral character in social work education. Social Work Education, 33(4), 451–468. https://doi.org/10.1080/02615479.2013.847914
Lindroth, M., Carlström, C., Andersson, C., & Husén, E. (2025). Social workers as allies? Gender confirming practices and institutional limitations in youth residential homes. Clinical Social Work Journal, 53(1), 108–116. https://doi.org/10.1007/s10615-024-00940-3
National Association of Social Workers. (2021). Code of ethics of the National Association of Social Workers. NASW. https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-Ethics-English
Raine, L. M., Vo, P., Wilson, S., Begay, P. L., & Drisko, J. (2023). What is clinical social work? Practitioners’ views. Clinical Social Work Journal, 51(4), 367–378. http://dx.doi.org/10.1007/s10615-023-00890-2
Contributor Biographies
Nafees Alam, PhD, LMSW, is a professor of social work and a licensed social worker who earned his doctorate at Yeshiva University. His research focuses on self-determination in sport social work, viewpoint diversity, open inquiry, and constructive disagreement in higher education. He has published extensively on these topics, including articles in Research on Social Work Practice, the Journal of Teaching in Social Work, and Psychology Today, as well as op-eds in Pulitzer Prize-winning outlets such as the Boston Herald and the Pittsburgh Post-Gazette. Dr. Alam has also contributed to initiatives promoting ideological diversity in academia through several organizations.
Chloe Carmichael, PhD, is a licensed clinical psychologist and USA Today bestselling author. She earned her doctorate in clinical psychology from Long Island University and a BA from Columbia University (summa cum laude, Phi Beta Kappa). She specializes in stress management, anxiety, self-esteem, and relationship issues. Dr. Carmichael is the author of Nervous Energy: Harness the Power of Your Anxiety and Can I Say That? Why Free Speech Matters and How to Use It Fearlessly. She serves on the advisory board of Women’s Health and has been featured in The New York Times, Forbes, and on national television.
Linda L. Chamberlain, PsyD, is a licensed psychologist and professor. She earned her doctorate at the University of Denver, School of Professional Psychology, in 1989, serving on the faculty there and later at the University of South Florida and Pasco–Hernando State College. She has written numerous books, including Practicing Psychotherapy: Lessons on Helping Patients and Growing as a Professional, and this year, she co-authored Psychotherapy in the Age of Political Polarization. Both books were published by Routledge. She serves as a co-moderator of the Mental Health Professionals Forum with Braver Angels, a volunteer organization with the mission of “bringing Americans together to bridge the partisan divide and strengthen our democratic republic.”
Matthew Fastman, PsyD, is a clinical psychologist specializing in evidence-based treatments for child anxiety. He completed his doctorate at Long Island University (LIU), C.W. Post, and has trained in leading clinics across New York, including New York-Presbyterian, Mount Sinai Hospital, and New York University Langone. He co-authored the first published study and clinician manual on independence therapy with Dr. Camilo Ortiz and continues to research independence therapy through grant-funded projects, including a large randomized controlled trial and a group-based intervention. He previously served as a researcher in LIU’s Applied Child Lab and led Safe Zone, a student initiative promoting LGBTQ+ clinical competence.
Andrew Hartz, PhD, is the founder and president of the Open Therapy Institute and a licensed psychologist. He was formerly a professor at Long Island University, where he completed his doctorate. He completed his clinical internship at Columbia University Medical Center and also trained at Mount Sinai Hospital and the William Alanson White Institute. For several years, Dr. Hartz has written about political issues and mental health for outlets such as The Wall Street Journal, City Journal, Discourse, The Federalist, RealClearEducation, Heterodox Academy, and The New York Post.
Kristopher Kaliebe, MD, is a professor and psychiatrist at the University of South Florida. Dr. Kaliebe is board certified in general psychiatry, forensic psychiatry, and child and adolescent psychiatry. A clinician, educator, and author, his academic and clinical interests include psychotherapy, mind–body medicine, the effects of technology on culture and mental health, overdiagnosis and overtreatment, and ideological influences on mental health care.
Neil J. Kressel, PhD, is a licensed psychologist and professor of psychology at William Paterson University, where he directed the honors program in the social sciences for 20 years. He holds a doctorate from Harvard and has taught at Harvard and New York University. Dr. Kressel was also a visiting associate professor at the Yale Initiative for the Interdisciplinary Study of Antisemitism. His textbook, The Psychology of Religion: A Social Force, was published by Cambridge University Press in 2024. His books on extremism include Mass Hate: The Global Rise of Genocide and Terror and “The Sons of Pigs and Apes”: Muslim Antisemitism and the Conspiracy of Silence.
William McCown, PhD, is a licensed clinical psychologist who earned his doctoral degree from Loyola University Chicago and interned at Tulane University Medical Center. He has served for more than 30 years as both professor and administrator at the University of Louisiana at Monroe. Dr. McCown has published research on gambling behavior, impulsivity, substance abuse, procrastination, family therapy, and chaos theory, among other areas, and he is the co-author of 10 books, including Psychotherapy in the Age of Political Polarization, published this year by Routledge.
Dean McKay, PhD, ABPP, is a professor of psychology at Fordham University and a licensed psychologist in New York, Connecticut, and Massachusetts. He completed his doctorate in clinical and school psychology at Hofstra University and is past president of the Association for Behavioral and Cognitive Therapies (2013–2014) and the Society for a Science of Clinical Psychology (2018). Dr. McKay has edited or co-edited 23 books. His expertise is in anxiety and obsessive-compulsive disorders, disgust in psychopathology, and misophonia (selective sound sensitivity), and he has recently expanded his research portfolio to include addressing antisemitism in medical and mental health care settings.
Stella O’Malley, MA, is an Ireland-based psychotherapist, author, and public speaker. She works in private practice with adolescents, young adults, and parents. O’Malley holds a master’s in cognitive behavioral therapy and a degree in counseling and psychotherapy, and she is currently completing a PhD on gender dysphoria in children and adolescents. She is the founder and executive director of Genspect and a frequent media contributor. She has authored several bestselling books, and The Gender Framework, a Genspect publication, will be published by Pitchstone Publishing later this year.
Douglas Novotny, PhD, is a clinical psychologist and educator based in California. He completed an interdisciplinary psychology doctorate at the University of Chicago and an internship at Cambridge Hospital. His specialties include child-family treatment, the interface between psychology and culture, natural horsemanship, and the life course of major individual philanthropists. Having trained and supervised therapists for 14 years, he recently founded Your Positive Sum LLC, which offers constructive solutions to culture war problems that corrode psychology as well as the values and institutions upon which the Western model of freedom and human flourishing is built.
Camilo Ortiz, PhD, ABPP, is an associate professor of psychology at Long Island University and the clinical director of the Open Therapy Institute. He is the co-developer of Independence Therapy, a novel treatment for child and adolescent anxiety. He also conducts research on parenting and disruptive behavior in children. Dr. Ortiz received a bachelor’s in human development from Cornell University and a PhD in clinical psychology from the University of Massachusetts Amherst. He is a partner at Cognitive Behavioral Associates, a group private practice on Long Island, New York.
Lawrence Ian Reed, PhD, is a clinical assistant professor at New York University. He earned his doctorate from the University of Pittsburgh and served as director of psychological services at McLean Hospital, Harvard Medical School. He is also co-chair of the New York University HxA Campus Community Network. His research on facial expression, emotion, and cooperation has resulted in multiple peer-reviewed academic papers. In addition, Dr. Reed specializes in treating adolescents and adults with mood disorders (e.g., depression and anxiety) and emotional disorders (e.g., borderline personality disorder).
William C. Sanderson, PhD, is a professor of psychology, director of clinical training, and director of the Anxiety & Depression Clinic at Hofstra University in New York. He is a founding fellow of the Academy of Cognitive Therapy and has served on numerous national committees, including the American Psychiatric Association’s DSM-IV Anxiety Disorders Workgroup. He has also served as editor of The Clinical Psychologist and as chair of the American Psychological Association Division of Clinical Psychology’s Committee on Science and Practice. Dr. Sanderson has published more than 100 articles, including seven books, primarily in the areas of anxiety, depression, evidence-based treatments, and cognitive behavior therapy.
Nina Silander, PsyD, is a clinical health psychologist, Regent University graduate, and an executive board member of the Society for Open Inquiry in Behavioral Science. She has contributed to books such as Cynical Therapies: Perspectives on the Antitherapeutic Nature of Critical Social Justice and Ideological and Political Bias in Psychology: Nature, Scope, and Solutions. Dr. Silander has published several academic articles as well as articles for the general public regarding sociopolitical biases in mental health care.
Val Thomas, DPsych, is a UK-based psychotherapist, writer, researcher, and former counselor educator. She has specialized in developing applications of mental imagery and has published two books with Routledge: Using Mental Imagery in Counselling and Psychotherapy and Using Mental Imagery to Enhance Creative and Work-Related Processes. In 2020, Dr. Thomas co-founded Critical Therapy Antidote, a platform for therapists concerned about the encroachments of critical social justice in the therapy field, and she edited the essay anthology Cynical Therapies: Perspectives on the Antitherapeutic Nature of Critical Social Justice.
Jaco van Zyl, MA, is a clinical psychologist and psychoanalytic psychotherapist in private practice in Ireland. He trained at Weskoppies Psychiatric Hospital and Kgoši Mampuru Correctional Services after qualifying at the University of Limpopo, South Africa. He is co-director of Critical Therapy Antidote (CTA), an organization examining the influence of critical social justice on mental health, and co-host of the CTA Podcast. He has published academic work and written for Merion West, Genspect, and Critical Therapy Antidote, and he is a contributor to an upcoming book on the psychodynamics of critical social justice.
















Thank you for this.
‘Dead to me’ is the corniest most melodramatic phrase when dealing with a difference of opinion. It’s the language of a bloated ego.
It’s intractability….
Don’t listen to these idiots.
Get around a fire, with your particular tipple, and jaw awhile.
We need to see that internally angry people suddenly found they had a voice and instead of using it well, they became everything they hated.
Tiresome bullies trying to ram their entitled beliefs into the quiet truths of everyday people trying to just get on with their lives.
Like Stonewalls tender claim that people who only wanted to be with the sex they were always attracted to were ‘sex racists’.
Or how about ‘kids know what is best for them’. ??
Right. Watch those lawsuits roll in. ‘But I was a kid !! How could you let me do that to myself!!? ‘.
And what do you say then?
What dodge will you use then?
The science isn’t settled.
The debate isn’t closed.
Lawyer up.